Addressing Surface Contamination in Biomedical Settings: Detection, Challenges, and Advanced Solutions
This article provides a comprehensive overview of surface contamination challenges in biomedical and pharmaceutical environments, with a focus on cytotoxic drug handling.
Addressing Surface Contamination in Biomedical Settings: Detection, Challenges, and Advanced Solutions
Abstract
This article provides a comprehensive overview of surface contamination challenges in biomedical and pharmaceutical environments, with a focus on cytotoxic drug handling. It explores the foundational risks to health and product integrity, details current and emerging methodological standards for detection, offers strategies for troubleshooting and optimizing decontamination procedures, and discusses validation and comparative analysis of monitoring technologies. Tailored for researchers, scientists, and drug development professionals, this review synthesizes the latest research, standards, and practical insights to enhance safety protocols, ensure regulatory compliance, and mitigate exposure risks in critical work environments.
Understanding the Spectrum and Impact of Surface Contaminants
Surface contamination represents a significant, yet often invisible, threat to experimental integrity, product safety, and occupational health in research and drug development environments. This threat spans multiple domains, from the palpable risk of cytotoxic drug exposure in hospital pharmacies to the subtle interference of trace elements in ultra-sensitive analytical procedures. Contaminants can be defined as any biological, chemical, or radiological substance unintentionally present on a surface that can compromise research results, harm personnel, or damage equipment. The central thesis of modern contamination control is that effective management requires a holistic strategy integrating advanced engineering controls, rigorous administrative procedures, and appropriate personal protective equipment. This technical support center provides targeted guidance to help researchers and scientists identify, troubleshoot, and prevent contamination issues, thereby safeguarding both their work and their well-being.
Troubleshooting Guides & FAQs
### FAQ: Cytotoxic Drug Handling
Q: What is the primary objective of a cytotoxic drug safety program? A: The main objective is to reduce the likelihood of accidental exposure to cytotoxic agents within the entire medication circuit, from the point the drugs enter the institution until they are administered to the patient or disposed of as waste [1]. The fundamental method for protecting workers follows a hierarchy of controls: elimination, substitution, engineering controls, administrative controls, and finally, personal protective equipment (PPE) [1].
Q: What personal protective equipment (PPE) is required for preparing solid oral cytotoxic drugs? A: For counting solid oral forms, personnel must wear a single pair of appropriate gloves. The risk of contamination with oral medications is considered minimal, but consistency in safety practices is crucial [1].
Q: Are there special considerations for pregnant staff handling cytotoxics? A: Yes. All staff should be fully informed of the potential reproductive hazards of cytotoxic drugs. The facility should strongly consider offering alternative duties for women who are pregnant or breast-feeding [1].
### FAQ: General Laboratory Contamination
Q: What are the most common sources of contamination in trace-level elemental analysis (e.g., ICP-MS)? A: The most frequent sources of contamination are [2]:
- Water: Impure water is a major source of ionic contamination.
- Acids and Reagents: Low-purity acids can introduce significant levels of trace elements.
- Labware: Glassware can leach boron, silicon, and sodium; improperly cleaned pipettes retain residues; and tubing can be a source of specific elemental contaminants.
- Laboratory Environment: Airborne dust, particulates from HVAC systems, and shedding from building materials.
- Personnel: Cosmetics, lotions, perfumes, jewelry, and even skin and hair can introduce contaminants.
Q: What is the difference between cleaning, disinfection, and sterilization? A: These represent different levels of decontamination [3] [4]:
- Cleaning: The necessary first step, which is the physical removal of organic matter, salts, and visible soils. This renders a surface safe to handle and is a form of decontamination.
- Disinfection: The process of inactivating most pathogenic microorganisms, but not necessarily all bacterial spores. Levels include high-level, intermediate-level, and low-level disinfection, based on the spectrum of microbes inactivated.
- Sterilization: The complete elimination or destruction of all forms of microbial life, including bacterial spores.
Q: How can I monitor the cleanliness of my surfaces? A: There is no single ideal method, and an integrated approach using trend analysis is recommended. Methods include [5]:
- Visual Inspection: Can be useful as part of an integrated approach but is ineffective in isolation.
- Non-microbial Methods: Adenosine Triphosphate (ATP) bioluminescence is highly effective at monitoring residual organic soil.
- Microbial Methods: Traditional microbial swabbing and contact plates indicate residual microbial contamination but not general surface soil.
### Troubleshooting Guide: Identifying Cell Culture Contaminants
The following table provides a quick-reference guide for identifying common biological contaminants in cell culture [6].
Table 1: Identification of Common Cell Culture Contaminants
| Contaminant | Visual & Microscopic Signs | Key Characteristics |
|---|---|---|
| Bacteria | Sudden pH change; cloudiness in medium; sometimes a slight whitish film. Under microscope (100x), granular appearance or small black dots between cells. | Can show motility. Can be distinguished from serum protein precipitates by their regular, particulate morphology. |
| Fungus (Mold) | Filamentous mycelia (thin, thread-like structures); denser clumps of spores. Overtakes a culture as a fuzzy white or black growth visible to the naked eye. | Usually slow-growing but can overwhelm a culture in advanced stages. |
| Yeast | Round or ovoid particles that are smaller than mammalian cells. Often seen as particles "budding" from each other in chains. | In advanced stages, can appear as multi-branched chains of particles. |
| Mycoplasma | No change visible to the naked eye or by standard light microscopy. | Requires specific detection methods (e.g., PCR, specialized agar cultivation showing "fried egg" colonies). |
Experimental Protocols for Contamination Assessment & Control
### Protocol 1: Assessing Surface Contamination by Cytotoxic Drugs
This protocol is adapted from a study evaluating contamination in hospital pharmacies and the efficacy of a closed-system drug-transfer device (CSTD) [7].
1. Objective: To establish baseline levels of surface contamination from intravenous cytotoxic drugs and to assess the effectiveness of an intervention (e.g., a CSTD) in reducing such contamination.
2. Materials:
- Berner International sampling kit or equivalent [7].
- Solvents for wiping (as per analytical method requirements).
- Sample vials and labels.
- Personal protective equipment (PPE) as defined in [1].
- Access to a validated analytical laboratory (e.g., using LC-MS/MS).
3. Sampling Methodology (Wipe Sampling):
- Sampling Time: Collect samples at the end of the day, before routine decontamination of the surfaces [7].
- Sampling Locations: Obtain wipe samples from defined critical surfaces. The European Society of Oncology Pharmacy (ESOP) protocol suggests [7]:
- Inside the biosafety cabinet (BSC)
- Floor in front of the BSC
- Gloves of personnel working under the BSC
- Door handle/knob inside the cleanroom
- Transportation box for ready-to-administer infusions
- Sampling Technique:
- Use a standard template to sample a defined area (e.g., 35 cm x 35 cm = 1225 cm²). If the surface is smaller, record the actual area [7].
- Moisten the wipe with an appropriate solvent.
- Wipe the defined area systematically in three different directions (e.g., horizontal, vertical, and diagonal) to maximize recovery [7].
- Fold the wipe, place it in a vial, seal, and freeze until analysis.
4. Experimental Design:
- Baseline Measurement: Perform wipe sampling across all designated locations before implementing any intervention.
- Post-Intervention Measurement: Implement the intervention (e.g., introduce a CSTD for all cytotoxic drug manipulations). After a predefined period (e.g., 2 weeks or 1 month), repeat the wipe sampling protocol in the exact same locations [7].
- Analysis: Samples are analyzed by a qualified laboratory (e.g., via LC-MS/MS) for a panel of target cytotoxic drugs (e.g., 5-fluorouracil, cyclophosphamide, docetaxel, etc.). Results are typically reported in nanograms per square centimeter (ng/cm²).
5. Data Interpretation:
- Compare the baseline and post-intervention levels for each drug and each surface using statistical tests (e.g., Wilcoxon test for paired samples) [7].
- A significant reduction in contamination levels post-intervention demonstrates the efficacy of the control measure.
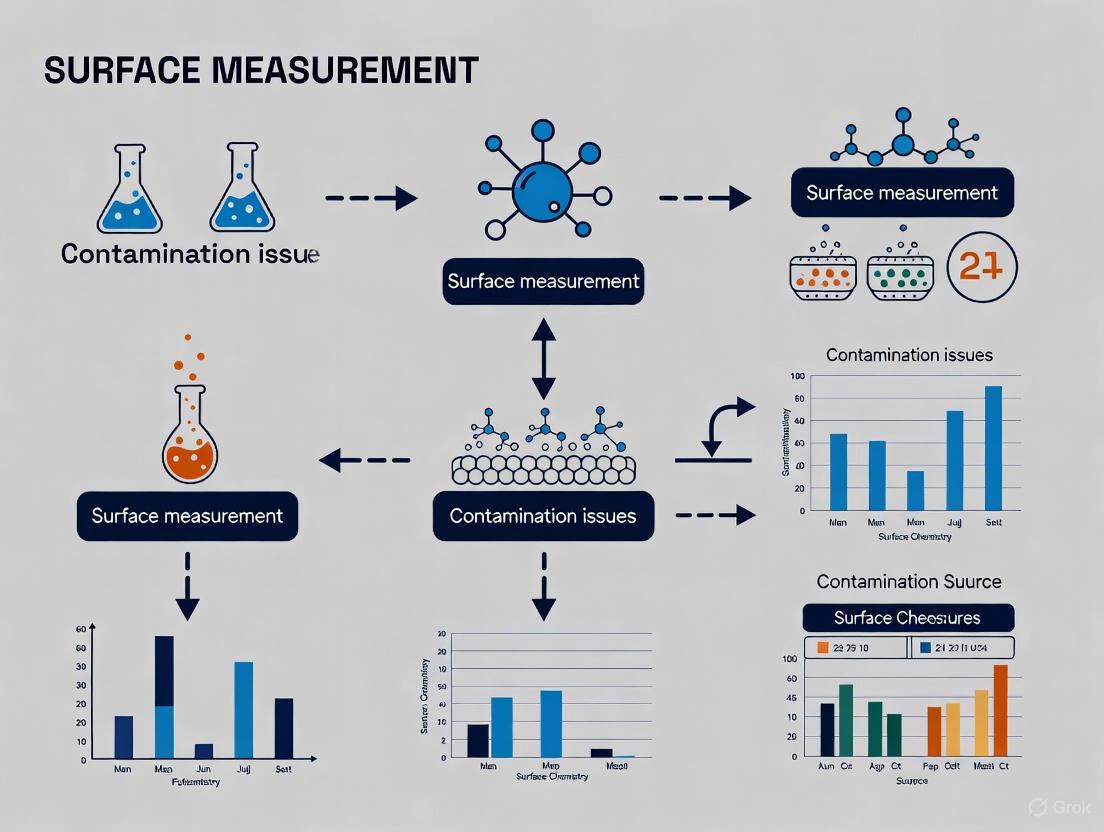
The following workflow diagram illustrates this experimental process.
### Protocol 2: Controlling Contamination in Trace Element Analysis (ICP-MS)
This protocol outlines best practices for minimizing background contamination during the preparation of samples and standards for ultra-trace elemental analysis [2].
1. Objective: To prepare samples and standards for ICP-MS analysis with minimal introduction of trace elemental contaminants from the laboratory environment, reagents, or labware.
2. Materials:
- Water: ASTM Type I or better ultrapure water [2].
- Acids: High-purity (e.g., ICP-MS grade) acids (nitric acid is relatively clean; hydrochloric acid often has higher impurities) [2].
- Labware: Fluorinated ethylene propylene (FEP) or quartz containers. Avoid borosilicate glass for analyses of B, Si, Na, etc. [2].
- Environment: Class 100 (or better) clean hood or cleanroom with HEPA filtration is ideal [2].
- Pipettes: Use dedicated, rigorously cleaned pipettes (automated pipette washers are highly effective) [2].
3. Methodology:
- Labware Preparation:
- Sample/Standard Preparation:
- Work in a clean hood whenever possible [2].
- Rinse the outside of all standard and sample containers with ultrapure water before opening to remove surface contamination [2].
- Recap all containers quickly after use to reduce environmental contamination [2].
- Prepare dilutions in FEP or other metal-free plastics [2].
- Use standard addition to compensate for complex sample matrices [2].
- Personnel Practices:
The Scientist's Toolkit: Essential Reagents & Materials
Table 2: Key Research Reagent Solutions for Contamination Control
| Item | Function & Rationale |
|---|---|
| Closed-System Drug-Transfer Device (CSTD) | A drug transfer device that mechanically prohibits the transfer of environmental contaminants into the system and the escape of hazardous drug or vapor concentrations outside the system. It is a critical engineering control for handling cytotoxic drugs [7]. |
| HEPA-Filtered Clean Hood / Biosafety Cabinet (BSC) | Provides a ISO Class 5 clean air environment for manipulating samples and standards, protecting them from airborne particulate contamination. A BSC also provides personnel and product protection for biohazardous work [1] [2]. |
| ASTM Type I Ultrapure Water | Water with the lowest possible levels of ionic and organic contaminants. It is essential for preparing blanks, standards, and samples in trace analysis to prevent contamination from the water itself [2]. |
| ICP-MS Grade Acids | Acids (e.g., HNO₃) certified to have extremely low levels of trace metal impurities. Using lower purity acids can introduce significant contamination that invalidates ultra-trace (ppb/ppt) measurements [2]. |
| Fluoropolymer (FEP) Labware | Containers and vessels made of FEP or similar plastics are inert and minimize leaching of trace elements and adsorption of analytes compared to glass or lower-quality plastics [2]. |
| Wipe-Sampling Kit | A standardized kit (e.g., Berner International kit) used for systematic surface sampling to quantify chemical contamination. Ensures consistent sampling area and technique for reliable data [7]. |
The decision-making process for selecting a decontamination method is guided by the nature of the contaminant and the required safety level, as shown in the following logic diagram.
Table 3: Efficacy of a Closed-System Drug Transfer Device (CSTD) in Reducing Cytotoxic Drug Contamination
This table summarizes quantitative results from a study conducted in 13 hospital pharmacies, showing the reduction in surface contamination (ng/cm²) after implementing a CSTD for a period of 2 weeks to 1 month [7].
| Cytotoxic Drug | Baseline Contamination Level | Post-Intervention Contamination Level | Efficacy of CSTD |
|---|---|---|---|
| 5-Fluorouracil (5-FU) | Detected | Reduced | Significantly Decreased |
| Cyclophosphamide | Detected | Reduced | Significantly Decreased |
| Docetaxel | Detected | Reduced | Significantly Decreased |
| Gemcitabine | Detected | Reduced | Significantly Decreased |
| Paclitaxel | Detected | Reduced | Significantly Decreased |
| Ifosfamide | Detected | Reduced | Significantly Decreased |
| Etoposide | Detected | Reduced | Data available in source [7] |
| Methotrexate | Detected | Reduced | Data available in source [7] |
Note: The study concluded that the use of the CSTD significantly decreased the contamination for 6 of the 8 compounds investigated. The level of contamination was generally higher at baseline than after the intervention [7].
Table 4: Impact of Laboratory Environment on Acid Purity (Contamination in ppb)
This table demonstrates the dramatic effect of the laboratory environment on the purity of reagents, comparing the levels of elemental contaminants in nitric acid distilled in a regular laboratory versus a HEPA-filtered cleanroom [2].
| Elemental Contaminant | Contamination in Regular Lab (ppb) | Contamination in Cleanroom (ppb) |
|---|---|---|
| Aluminum (Al) | High | Significantly Lower |
| Calcium (Ca) | High | Significantly Lower |
| Iron (Fe) | High | Significantly Lower |
| Sodium (Na) | High | Significantly Lower |
| Magnesium (Mg) | High | Significantly Lower |
Note: The study showed that the acid distilled in the regular laboratory had high amounts of contamination, while the acid distilled in the clean room showed significantly lower amounts of most contaminants [2].
Hospitals are among the most hazardous places to work, with U.S. hospitals recording 221,400 work-related injuries and illnesses in 2019 alone—a rate nearly double that of private industry as a whole [8]. For researchers and drug development professionals investigating surface contamination, understanding the risks posed by Hazardous Medicinal Products (HMOs) is critical. These substances, including antineoplastic drugs, immunosuppressants, and antiviral medicines, present significant carcinogenic, mutagenic, and reprotoxic risks to healthcare workers during preparation, administration, and cleanup [9]. Recent regulatory updates, including the expanded EU Directive 2004/37/EC, now explicitly address these risks with an indicative list of HMPs and mandated safety protocols [9]. This technical support center provides methodologies, troubleshooting guides, and FAQs to support your research into detecting and measuring these hazardous contaminants on surfaces.
Experimental Protocols: Detection of Surface Contamination
Multiplexed Fluorescence Covalent Microbead Immunosorbent Assay (FCMIA)
The FCMIA technique enables simultaneous detection and semi-quantitative measurement of multiple antineoplastic drugs from surface samples, providing a cheaper and faster alternative to traditional LC-MS/MS methods [10].
The diagram below illustrates the FCMIA experimental workflow for detecting surface contamination of antineoplastic drugs:
Detailed Methodology
Surface Sampling Protocol
- Wipe the test surface with a swab wetted with wash buffer (phosphate buffered saline [PBS], 138 mM NaCl, 2.7 mM KCl, containing 0.05% Tween 20)
- Extract the swab in storage/blocking buffer (PBS, 1% BSA, 0.05% NaN3, pH 7.4)
- Analyze the extract using FCMIA [10]
Microsphere Preparation
- Use 5.6μm carboxylate-modified microspheres with internal red and infrared fluorochromes
- Activate carboxylate groups with EDC and NHS in activation buffer (0.1 M NaH2PO4, pH 6.2)
- Couple drug-BSA conjugates (5-fluorouracil-BSA, doxorubicin-BSA, paclitaxel-BSA) to unique microsphere sets in coupling buffer (0.05 M MES, pH 5.0) [10]
Multiplexed Assay Procedure
- Perform competitive assay in 1.2μm filter membrane microtiter plates
- Incubate with primary anti-drug monoclonal antibodies
- Add biotin-labeled anti-mouse IgG secondary antibody
- Bind streptavidin R-phycoerythrin fluorescent label
- Analyze using LUMINEX 100 instrument, collecting data from 100 microspheres per analyte
- Determine median fluorescence intensity (MFI) for quantification [10]
Standard Curves and Quantification
Prepare standard solutions at 8 concentrations for calibration as shown in the table below:
Table 1: Standard Solution Concentrations for FCMIA Calibration
| Standard Solution | 5-Fluorouracil (ng/mL) | Paclitaxel (ng/mL) | Doxorubicin (ng/mL) |
|---|---|---|---|
| 1 | 1000 | 100 | 2 |
| 2 | 500 | 50 | 1 |
| 3 | 250 | 25 | 0.5 |
| 4 | 125 | 12.5 | 0.25 |
| 5 | 62.5 | 6.25 | 0.125 |
| 6 | 31.25 | 3.125 | 0.0625 |
| 7 | 15.6 | 1.5625 | 0.0312 |
| 8 | 0 | 0 | 0 |
Construct standard curves using four-parameter logistic-log fits for quantification of unknown samples [10].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Antineoplastic Drug Detection
| Reagent/Material | Function | Example Sources |
|---|---|---|
| Carboxylate-modified microspheres | Solid support for covalent attachment of biomolecules; enable multiplexing through internal fluorochromes | Luminex Corporation |
| Drug-BSA conjugates (5-fluorouracil-BSA, doxorubicin-BSA, paclitaxel-BSA) | Capture antigens for competitive immunoassay | Saladax Biomedical |
| Monoclonal anti-drug antibodies | Primary antibodies for specific drug detection | Saladax Biomedical, Lampire Biological Laboratories |
| EDC and Sulfo-NHS | Activation of carboxylate groups on microspheres for biomolecule coupling | Pierce Biotechnology, Inc. |
| Biotin-labeled anti-mouse IgG | Secondary antibody for signal amplification | Pierce Biotechnology, Inc. |
| Streptavidin R-phycoerythrin | Fluorescent label for detection | Molecular Probes |
| Filter membrane microtiter plates | Platform for assay with built-in wash capabilities | Millipore Corp. (MABVN1250) |
Safety Protocols and Regulatory Framework
Recent EU OSHA updates (Directive 2004/37/EC) establish significant new requirements for handling Hazardous Medicinal Products (HMPs) with carcinogenic, mutagenic, or reprotoxic properties [9].
Employer Responsibilities and Safety Systems
The diagram below outlines the comprehensive safety approach required for HMP handling:
Key Regulatory Changes
Addition of Reprotoxic Substances: Reprotoxic substances are now fully recognized under the CMR framework, amplifying protection for workers handling substances linked to fertility issues, birth defects, or developmental disorders [9]
Indicative List of HMPs: First EU-endorsed indicative list includes antineoplastics, immunosuppressants, and antiviral medicines classified as Category 1A or 1B carcinogens, mutagens, or reprotoxic agents [9]
Expanded Employer Obligations: Mandates for robust safety protocols including regular worker training, detailed risk assessments, substitution of hazardous substances where feasible, and use of closed systems to prevent exposure [9]
Performance Data and Detection Limits
Table 3: FCMIA Detection Limits for Antineoplastic Drugs
| Antineoplastic Drug | Limit of Detection (LOD) (ng/cm²) | Limit of Quantitation (LOQ) (ng/cm²) | Commercial Preparation Concentration |
|---|---|---|---|
| 5-Fluorouracil | 0.93 | 2.8 | 50 mg/mL |
| Paclitaxel | 0.57 | 2.06 | 6 mg/mL |
| Doxorubicin | 0.0036 | 0.013 | 2 mg/mL |
The extreme sensitivity of the FCMIA method is particularly valuable given the high concentration of commercial drug preparations, where even minimal spillage can cause significant contamination [10].
Troubleshooting Guides and FAQs
Common Experimental Challenges
Q: We're observing high background signal in our FCMIA results. What could be causing this and how can we address it?
A: High background often stems from incomplete washing steps or nonspecific antibody binding. Ensure thorough washing between assay steps using appropriate wash buffer (PBS with 0.05% Tween 20). Optimize antibody concentrations and include appropriate controls. Verify that your storage/blocking buffer (PBS, 1% BSA, 0.05% NaN3) is fresh and properly prepared [10].
Q: Our surface recovery rates for antineoplastic drugs are inconsistent. How can we improve sampling reliability?
A: Standardize your swabbing technique using consistent pressure and pattern. Ensure swabs are adequately wetted with wash buffer but not oversaturated. For porous surfaces, increase sampling area. Extract swabs immediately after collection and analyze promptly to prevent degradation. Validate your recovery efficiency for different surface types [10].
Q: What are the critical safety thresholds for surface contamination of antineoplastic drugs in healthcare settings?
A: While regulatory standards for surface contamination are still evolving, your research should aim for detection of less than 1 ng/cm² and measurement of less than 5 ng/cm² for multiple antineoplastic drugs. These levels are useful in assessing contamination to control exposure, particularly given that studies show workplace contamination persists despite safe handling practices [10].
Regulatory and Compliance FAQs
Q: How do the recent EU OSHA updates affect our research on surface contamination of HMPs?
A: The 2025 EU OSHA update establishes an indicative list of HMPs and emphasizes closed systems for exposure prevention. Your research should align with these guidelines by validating detection methods for the listed HMPs and evaluating the effectiveness of engineering controls like Closed System Transfer Devices (CSTDs). Reference the official indicative list (COMMUNICATION FROM THE COMMISSION, C/2025/1150) in your methodology [9].
Q: What health surveillance data should we collect to correlate with surface contamination findings?
A: Studies reveal nurses handling cytotoxic drugs are three times more likely to develop malignancies compared to those not exposed. Collect data on short-term health effects (skin irritation, respiratory issues) and long-term outcomes (cancer incidence, reproductive issues) while maintaining participant confidentiality. Correlate this with both personal exposure monitoring and surface contamination data [9].
The detection and measurement of surface contamination by hazardous drugs represents a critical component of protecting healthcare workers from carcinogenic, mutagenic, and reproductive hazards. The FCMIA methodology provides researchers with a sensitive, specific, and practical approach for simultaneous detection of multiple antineoplastic drugs. As regulatory frameworks evolve to address these risks, your research plays a vital role in establishing evidence-based safety protocols and contamination control measures. By implementing these methodologies and troubleshooting guides, you contribute to the broader thesis of addressing contamination problems in surface measurements research while enhancing workplace safety for healthcare professionals.
Frequently Asked Questions (FAQs)
Q1: What do recent surveillance data indicate about respiratory virus activity in healthcare settings? Recent data from England (May 2025) shows respiratory viruses circulating at baseline levels. COVID-19 PCR positivity in hospital settings was 5.6%, influenza positivity was 1.5%, and RSV positivity was 0.2%. These figures help researchers contextualize the background prevalence of viruses that could potentially contaminate surfaces in medical environments [11].
Q2: How sensitive are modern methods for detecting surface contamination by antineoplastic drugs? Fluorescence Covalent Microbead Immunosorbent Assay (FCMIA) can simultaneously detect multiple drugs with high sensitivity. Limits of Detection (LOD) for common agents are:
- Doxorubicin: 0.0036 ng/cm²
- Paclitaxel: 0.57 ng/cm²
- 5-Fluorouracil: 0.93 ng/cm² This sensitivity is crucial for monitoring hazardous drug residues on work surfaces [10].
Q3: What is a cost-effective approach for ongoing surveillance of pathogen prevalence? Studies comparing surveillance systems found that lower-cost methods like the Virus Watch study (costing £4.89 million) can effectively track positivity and incidence rates, showing strong synchrony (Spearman ⍴: 0.90-0.92) with more expensive, gold-standard systems like the ONS COVID-19 Infection Survey (costing £988.5 million). This demonstrates that robust surveillance is possible in resource-limited settings [12].
Table 1: Recent Respiratory Virus Positivity Rates in Hospital Settings (England, May 2025)
| Virus | Positivity Rate | Trend | Hospital Admission Rate (per 100,000) |
|---|---|---|---|
| COVID-19 | 5.6% (PCR) | Stable | 1.38 |
| Influenza | 1.5% (weekly mean) | Decreasing | 0.37 |
| RSV | 0.2% | Stable | Reporting concluded |
| Rhinovirus | 12.1% | Stable | Not specified |
| Adenovirus | 3.8% | Decreasing slightly | Not specified |
| hMPV | 1.7% | Decreasing | Not specified |
Source: UK Health Security Agency National Flu and COVID-19 Surveillance Report [11]
Table 2: Detection Limits for Antineoplastic Drug Surface Contamination Using FCMIA
| Antineoplastic Drug | Limit of Detection (LOD)(ng/cm²) | Limit of Quantitation (LOQ)(ng/cm²) | Commercial Preparation Concentration |
|---|---|---|---|
| Doxorubicin | 0.0036 | 0.013 | 2 mg/ml |
| Paclitaxel | 0.57 | 2.06 | 6 mg/ml |
| 5-Fluorouracil | 0.93 | 2.8 | 50 mg/ml |
Source: Journal of Oncology Pharmacy Practice [10]
Experimental Protocols
Protocol 1: Multiplexed Surface Detection of Antineoplastic Drugs Using FCMIA
Purpose: Simultaneous detection and semi-quantitative measurement of multiple antineoplastic drugs on workplace surfaces [10].
Materials:
- Carboxylate-modified microspheres (5.6 μm diameter)
- Drug-BSA conjugates (5-fluorouracil-BSA, doxorubicin-BSA, paclitaxel-BSA)
- Monoclonal antibodies specific to each drug
- Biotin-labeled anti-mouse IgG
- Streptavidin R-phycoerythrin
- EDC and sulfo-NHS in activation buffer (0.1 M NaH₂PO₄, pH 6.2)
- Coupling buffer (0.05 M MES, pH 5.0)
- Storage/blocking buffer (PBS, 1% BSA, 0.05% NaN₃, pH 7.4)
Methodology:
- Surface Sampling: Wipe the measured surface area with a swab wetted with wash buffer.
- Sample Extraction: Extract the swab in storage/blocking buffer.
- Microsphere Preparation: Activate carboxylate groups on microspheres with EDC/NHS mixture. Covalently couple each drug-BSA conjugate to unique microsphere sets.
- Multiplexed Assay: Perform competitive assay where drugs in sample extracts compete with microsphere-bound drug-BSA conjugates for anti-drug antibodies.
- Detection: Incubate with biotin-labeled secondary antibody followed by streptavidin R-PE.
- Analysis: Analyze using Luminex instrument; measure median fluorescence intensity (MFI). Decreased signal indicates higher drug concentration.
Typical Analysis Time: <15 minutes from sampling to results [10].
Protocol 2: Low-Cost Community Surveillance for Pathogen Positivity Rates
Purpose: Estimate community positivity and incidence rates using a cost-effective methodology [12].
Materials:
- Online survey platform (e.g., REDCap)
- Access to national testing data (where available)
- Participant recruitment materials
- Data linkage agreements with health authorities
Methodology:
- Participant Recruitment: Enroll households with internet access and ability to complete regular surveys (English proficiency required).
- Data Collection: Collect self-reported symptom data, test results, and demographic information through regular surveys.
- Data Linkage: Where possible, link participant data to national COVID-19 testing, vaccination, and hospital admission records.
- Rate Calculation: Calculate positivity rates from both self-reported and linked national testing data.
- Validation: Compare rate estimates with gold-standard surveillance systems using Spearman correlation for global and local synchrony.
Experimental Workflow Visualization
Surface Contamination Analysis Workflow
Surveillance System Validation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Surface Contamination Research
| Research Reagent | Function | Application Example |
|---|---|---|
| Carboxylate-Modified Microspheres | Solid support for covalent attachment of biomolecules; internally dyed for spectral addressability | Multiplexed detection of multiple analytes simultaneously in FCMIA [10] |
| Drug-BSA Conjugates | Immobilized antigens that compete with sample analytes for antibody binding | Critical for competitive immunoassay format used in surface contamination detection [10] |
| Monoclonal Antibodies | Specific recognition elements that bind target analytes with high affinity | Enable specific detection of individual antineoplastic drugs in complex samples [10] |
| Biotin-Labeled Secondary Antibodies | Amplification reagents that bind primary antibodies | Signal enhancement in immunochemical detection methods [10] |
| Streptavidin R-Phycoerythrin | Fluorescent reporter for detection and quantification | Provides measurable signal proportional to analyte concentration in FCMIA [10] |
| EDC and Sulfo-NHS | Cross-linking agents for covalent immobilization | Activation of carboxylate groups on microspheres for biomolecule conjugation [10] |
| Linked National Testing Data | Validation and enhancement of self-reported infection data | Improves accuracy of positivity rate estimates in surveillance studies [12] |
Troubleshooting Guides and FAQs for Surface Contamination Research
This technical support center addresses common experimental challenges in surface contamination measurement, framed within a broader thesis on amending contamination problems in surface measurements research.
Troubleshooting Common Experimental Issues
FAQ 1: Our surface sampling for antineoplastic drugs shows inconsistent results between replicates. What are the potential causes?
- Potential Causes & Solutions:
- Inconsistent Swab Technique: The pressure, pattern, and wetness of the swab during surface sampling must be standardized. A common method is to wipe the entire surface with a swab wetted with wash buffer, using a consistent, overlapping "S" pattern while applying firm, even pressure [10].
- Incomplete Surface Extraction: After sampling, the swab must be properly extracted in an appropriate storage/blocking buffer to ensure the analyte is fully released for measurement [10].
- Cross-Contamination of Samples: Ensure that fresh swabs are used for each sample and that gloves are changed between replicates to prevent carry-over contamination [13].
- Degraded Reagents: Check the expiry dates of all reagents, including antibodies, fluorescent labels, and buffer solutions. Using reagents past their expiry can lead to diminished assay signals and unreliable data [13].
FAQ 2: We are detecting microbial contamination on surfaces that appear visually clean. How should we interpret this, and what are the next steps?
- Interpretation & Next Steps:
- Interpretation: Visually clean surfaces can still be heavily contaminated. Low or undetectable pathogen concentrations on high-touch surfaces should not be interpreted as an absence of pathogen spread via surface touch. These surfaces can act as key nodes with high 'flux,' facilitating microbial transmission despite moderate contamination levels [14].
- Next Steps:
- Review Cleaning Protocols: Ensure that cleaning is always performed before disinfection, as dirt and organic matter can shield microorganisms [13] [15].
- Validate Disinfectant Contact Time: Confirm that the disinfectant remains wet on the surface for the entire manufacturer-recommended contact time to achieve effective kill [13] [15].
- Evaluate Sporicidal Use: In critical environments, incorporate a sporicidal agent into the disinfection rotation to control resilient pathogens like C. difficile [13] [16].
FAQ 3: Our environmental monitoring in a cleanroom is consistently failing due to airborne particulate matter. What areas should we investigate?
- Investigation Checklist:
- Gowning Procedures: Re-train personnel on aseptic gowning practices. Failure to don gowns, gloves, and hair covers correctly is a primary source of human-shed particulates [13].
- Material Transfer: Verify that all materials entering the cleanroom are properly disinfected at the point of transition from a lower-classified area to a higher-classified area [13].
- Facility Integrity: Inspect the room for insanitary conditions, including unsealed or loose ceiling tiles, damaged wall panels, and standing water, all of which can contribute to particulate shedding and microbial growth [13].
- Equipment: Audit equipment brought into the cleanroom to ensure it is non-porous, non-particle-generating, and easy to clean [13].
Experimental Protocols for Surface Measurement
Protocol: Multiplexed Measurement of Surface Contamination by Antineoplastic Drugs using FCMIA
This protocol enables simultaneous detection and semi-quantitative measurement of multiple antineoplastic drugs (e.g., 5-fluorouracil, paclitaxel, doxorubicin) from surfaces [10].
1. Principle A fluorescence covalent microbead immunosorbent assay (FCMIA) is used. In this competitive immunoassay, drug residues extracted from a surface compete with drug-protein conjugates immobilized on color-coded microspheres for a limited amount of anti-drug antibody. The signal detected is inversely proportional to the amount of drug present on the surface [10].
2. Materials and Reagents
- Drug-BSA Conjugates: 5-fluorouracil-BSA, doxorubicin-BSA, paclitaxel-BSA.
- Monoclonal Antibodies: Specific to each target drug.
- Carboxylated Microspheres: Different sets with unique internal fluorescent signatures.
- Coupling Buffers: Activation buffer (0.1 M NaH2PO4, pH 6.2) and coupling buffer (0.05 M MES, pH 5.0).
- Assay Buffers: Wash buffer (PBS with 0.05% Tween 20) and storage/blocking buffer (PBS with 1% BSA and 0.05% NaN3).
- Detection Reagents: Biotin-labeled anti-mouse IgG and Streptavidin R-Phycoerythrin (Streptavidin R-PE).
- Sampling Kit: Swabs and containers for surface sampling.
- Luminex Instrumentation: A flow-based system, such as a LUMINEX 100, for reading the multiplexed assay.
3. Procedure
- Surface Sampling: Wipe the target surface systematically with a swab wetted with wash buffer. Extract the swab in storage/blocking buffer [10].
- Microsphere Coupling (if required): Covalently couple each drug-BSA conjugate to a unique set of activated microspheres using EDC and NHS chemistry [10].
- Multiplexed Assay Execution:
- Incubate the sample extract with a mixture of conjugated microspheres and primary anti-drug antibodies.
- Wash to remove unbound components.
- Incubate with biotin-labeled secondary antibody.
- Wash again.
- Incubate with Streptavidin R-PE.
- Perform a final wash and resuspend the microspheres for reading.
- Data Acquisition and Analysis: The Luminex instrument reads the internal fluorescence of each microsphere to identify it and measures the median fluorescence intensity (MFI) of the surface-bound R-PE. Standard curves are generated from known drug concentrations, and sample concentrations are interpolated from these curves [10].
4. Expected Results and Limits of Detection The following limits of detection (LOD) and quantitation (LOQ) have been achieved for this method on the surfaces studied [10]:
Table 1: Assay Sensitivity for Key Antineoplastic Drugs
| Drug | Limit of Detection (LOD) (ng/cm²) | Limit of Quantitation (LOQ) (ng/cm²) |
|---|---|---|
| 5-Fluorouracil | 0.93 | 2.8 |
| Paclitaxel | 0.57 | 2.06 |
| Doxorubicin | 0.0036 | 0.013 |
Workflow Visualization: FCMIA for Surface Contamination
The following diagram illustrates the core workflow and principle of the FCMIA for detecting surface contamination.
The Scientist's Toolkit: Research Reagents & Materials
Table 2: Essential Materials for Surface Contamination Research via FCMIA
| Item | Function / Application |
|---|---|
| Drug-BSA Conjugates | Conjugated proteins immobilized on microspheres to capture specific antibodies in the competitive FCMIA [10]. |
| Monoclonal Antibodies | Bind specifically to target drug analytes; the key reagent determining assay specificity [10]. |
| Carboxylated Microspheres | Solid support with internal color-coding for multiplexing and surface carboxyl groups for biomolecule conjugation [10]. |
| Biotin-labeled Anti-IgG | Secondary antibody that binds to the primary drug-specific antibody, enabling signal amplification via streptavidin [10]. |
| Streptavidin R-Phycoerythrin | Fluorescent reporter that binds to biotin, producing the measurable signal for quantification [10]. |
| Sporicidal Disinfectant | A disinfectant effective against bacterial spores (e.g., chlorine-based) used to decontaminate surfaces and control pathogens like C. difficile in experimental settings [13] [16]. |
| High-Touch Surface Markers | Not a reagent, but a critical reference. Common high-touch surfaces (bed rails, IV poles, bedside tables) are key study targets for contamination mapping and sampling [17] [16]. |
Implications for Product Integrity and Cross-Contamination in Sensitive Manufacturing
Troubleshooting Guides and FAQs
What are the most common root causes of cross-contamination in a manufacturing environment?
The most common root causes can be categorized by their origin [18] [19]:
- Human Handling: Operators can transfer contaminants via dirty hands or contaminated clothing [18].
- Shared Equipment: Using the same machine or utensils for different products without proper cleaning is a frequent cause [18].
- Ineffective Cleaning: This includes inefficient use of cleaning agents, ineffective application of sanitation principles, and the presence of difficult-to-clean "niche environments" in equipment where bacteria can thrive [20].
- Environmental Factors: Airborne particles can transport contaminants, and work surfaces not disinfected between batches pose a risk [18].
- Raw Materials: Ingredients can be a source of contamination if stored together without proper separation or received from non-compliant suppliers [18].
Why might our current cleaning protocols be failing, even when followed?
Your protocols might be failing due to several subtle reasons [20]:
- Niche Environments: Bacteria can establish in sites like hollow conveyor rollers, cracked seals, or between close-fitting parts that are impossible to reach with normal cleaning [20].
- Biofilms: Bacteria can form slime layers on surfaces that protect them from conventional cleaning and sanitizing methods. Adequate physical cleaning to remove biofilms prior to sanitation is crucial [20].
- Ineffective Training: Training may be too generic, language barriers may exist, or the wrong personnel may be trained, reducing the effectiveness of cleaning execution [20].
- Poor Equipment Design: Equipment that lacks sanitary design, with materials that are not easily cleanable or parts that are not readily accessible, can undermine cleaning efforts [20].
We regularly test high-touch surfaces and find low pathogen levels. Does this mean the risk of contamination spread is low?
Not necessarily. A key node in microbial dissemination can exhibit moderate or even low contamination levels because they are frequently touched [14]. The high frequency of touch means these surfaces have a high "flux"—they can either contaminate a clean hand or be "cleaned" by a clean hand. Therefore, undetectable or low pathogen concentrations on high-touch surfaces should not be interpreted as an absence of risk for pathogen spread via surface touch [14].
What advanced methods can detect contamination that is invisible to the human eye?
Optical imaging methods using safe visible light, such as hyperspectral scanning, show promise. This technique can reveal human-eye invisible stains by utilizing the intrinsic fluorescence properties of biological contaminants and organic soils [21]. These systems use algorithms, including machine learning, to detect contamination "fingerprints" in the electromagnetic spectrum, allowing for real-time cleanliness evaluation [21].
Contaminant Types and Control Measures
The table below summarizes the primary categories of contaminants and methods to control them, drawing from food and pharmaceutical manufacturing principles [22].
| Contaminant Type | Common Examples | Primary Control Measures |
|---|---|---|
| Chemical | Pesticides, cleaning agents, lubricants, allergen residues [20] [22] | Regular equipment checks and maintenance; proper rinsing/cleaning validation; supplier verification and ingredient testing [22]. |
| Physical | Metal fragments, plastic, wood, pest-related matter [22] | Use of X-rays, metal detectors, sifting; Good Manufacturing Practices (GMPs); a food defense plan [22]. |
| Microbial | Pathogenic bacteria (e.g., L. monocytogenes), viruses, molds [20] [22] | Comprehensive sanitation protocols; employee hygiene training; environmental monitoring; product testing [22]. |
| Allergenic | Unintended transfer of allergenic ingredients (e.g., peanuts, milk) [22] | Segregation of processing environments and utensils; proper sanitization between production runs [22]. |
Experimental Protocol: Hyperspectral Imaging for Surface Cleanliness Monitoring
This protocol is adapted from a study conducted in a real-life hospital environment to detect organic dirt and biological contamination on touch surfaces [21].
Objective
To utilize hyperspectral imaging to detect visible and invisible stains on touch surfaces, correlating findings with culturable bacteria and ATP counts.
Materials and Equipment
- Hyperspectral imaging system (e.g., AutoDet) operating in the visible light spectrum (e.g., 420–720 nm) [21].
- Sterile swabs for microbiological sampling.
- ATP monitoring system (e.g., Ultrasnap swabs and luminometer) [21].
- Trypticase Soy Agar plates and selective agar plates for indicator bacteria [21].
- Surfaces for testing (e.g., chair armrests, door handles, lock knobs).
Methodology
- Sampling Site Selection: Identify diverse high-touch and low-touch surfaces in the facility. Sample on days representing a "worst-case scenario" (e.g., before the first cleaning of the week) [21].
- Optical Measurement: Use the hyperspectral imager to scan the target surface. Perform scans on both dirty and subsequently cleaned surfaces for comparison.
- Manual Algorithm: Use threshold levels for intensity and clustering analysis with specific excitation lights (e.g., green, red) and bandpass filters (e.g., λ = 500 nm) [21].
- Automatic Algorithm: Employ machine vision algorithms like k-means clustering on data from the entire visible light spectrum (red, green, blue) and filters from 420 to 720 nm at 20 nm increments [21].
- Microbiological Validation:
- Perform swap wiping on the same surface area.
- Analyze for Total Plate Count (TPC) using Trypticase Soy Agar.
- Test for specific indicator bacteria (e.g., S. aureus, Enterococci, Gram-negatives) using selective agar plates and enrichment steps [21].
- Organic Soil Validation:
- Collect a dry swab sample for ATP measurement.
- Express results in Relative Light Units (RLU) per unit area [21].
- Data Analysis: Correlate the optical imaging results with the microbiological and ATP data. A successful detection is confirmed when the imaging system reveals a stain that correlates with high TPC or ATP counts, even if it was invisible to the naked eye [21].
The Scientist's Toolkit: Key Research Reagent Solutions
| Item or Solution | Function / Explanation |
|---|---|
| Adenosine Triphosphate (ATP) Monitoring System | Provides a rapid estimate of total organic soil (both microbial cells and food/residues) on a surface. It is fast but unspecific for pathogens [21]. |
| Hyperspectral Imaging System | Allows for non-contact, real-time monitoring of surface cleanliness by detecting the unique spectral "fingerprints" of organic and biological contaminants, including those invisible to the eye [21]. |
| Selective Culture Media | Used to isolate and identify specific indicator bacteria (e.g., Enterococcosel Agar for Enterococci, Mannitol Salt Agar for S. aureus), confirming the type of microbial contamination [21]. |
| Validated Cleaning Agents & Disinfectants | Chemical solutions whose efficacy against target microbes has been confirmed for specific soil types, contact times, and concentrations in the given environment [20]. |
| Microbiological Swabs | Tools for aseptically collecting samples from surfaces for subsequent cultivation or molecular analysis, enabling the quantification and identification of viable microbes [21]. |
Contamination Spread and Control Workflow
Cross-Contamination Control Strategy
Advanced Techniques and Standards for Contamination Detection and Monitoring
Troubleshooting Guides
FAQ: How Can I Improve the Sensitivity of My LC-MS/MS Method?
Answer: Sensitivity in LC-MS/MS is a function of the signal-to-noise ratio (S/N). Improvements can be made by boosting the analyte signal and by reducing background noise and contaminants. Key strategies involve optimizing the mass spectrometer's source parameters, carefully selecting mobile phases and additives, and employing rigorous sample preparation to minimize matrix effects [23].
Critical MS Source Parameters for ESI Optimization: The following parameters should be optimized for your specific analyte, mobile phase, and flow rate [23].
| Parameter | Influence on Sensitivity | Optimization Guidance |
|---|---|---|
| Capillary Voltage | Maintains stable spray; affects ionization efficiency [23]. | Set to match analytes, eluent, and flow rate; incorrect settings cause variable ionization and poor precision [23]. |
| Nebulizing Gas Flow & Temperature | Affects droplet size and charge accumulation [23]. | Increase for faster flow rates or highly aqueous mobile phases [23]. |
| Desolvation Gas Flow & Temperature | Critical for producing gas-phase ions [23]. | Increase for effective desolvation; use caution with thermally labile analytes to prevent degradation [23]. |
| Capillary Tip Position | Impacts ion plume density and transmission into the MS [23]. | Place further from orifice at high flow rates; closer at slower flow rates to increase ion plume density [23]. |
FAQ: Why is There High Background Noise or Unidentified Peaks in My Chromatograms?
Answer: High background signals are frequently caused by contaminants introduced from solvents, additives, samples, or the analyst themselves. These contaminants increase baseline noise, can interfere with the detection of target analytes, and cause ion suppression or enhancement, leading to quantitative inaccuracies [24].
Common Contaminant Sources and Solutions:
| Source Category | Examples of Contaminants | Preventive Measures |
|---|---|---|
| Solvents & Additives | Microbial growth, solvent impurities, leachates from filters, residual detergents [24]. | Use HPLC-MS grade solvents; avoid unnecessary filtering; dedicate solvent bottles; test different additive sources [24]. |
| Samples & Preparation | Keratins (skin, hair), lipids, plasticizers from tubes/vials, sample carryover [24]. | Wear nitrile gloves; use high-quality consumables; employ thorough cleaning protocols [24]. |
| Instrumentation | Compounds from inlet filters/lines, leachates from polymer seals [24]. | Handle solvent lines with care; use instrument-specific components; flush with organic solvent during extended idle periods [24]. |
FAQ: How Can I Better Detect Low-Abundance Compounds or Handle Non-Ideal Peak Shapes?
Answer: Traditional methods relying on intensity thresholds or rigid mathematical peak-shape models often miss low-abundance compounds or those with non-ideal distributions. A modern solution is to use deep learning-based feature detection algorithms, such as SeA-M2Net, which treat feature detection as an image-based object detection task. This method learns the distribution difference between compounds and noise directly from 2D pseudo-color images of the LC-MS data, allowing it to detect low-abundance and overlapping compounds with high robustness without pre-defined shape assumptions [25].
Experimental Protocol for Deep Learning Feature Detection (SeA-M2Net):
- Data Transformation: Convert raw LC-MS data into a 2D data matrix based on retention time (RT) and mass-to-charge (m/z) dimensions [25].
- Image Generation: Generate a 2D pseudo-color image from the data matrix, where the color intensity represents the abundance of the ions. This integrates visual features like LC elution, charge state, and isotope distribution [25].
- Model Application: Process the image using the pre-trained SeA-M2Net deep convolutional neural network. The network uses a deep multilevel and multiscale structure to estimate the probability of a compound's presence [25].
- Output: The algorithm provides probability outputs (compound vs. noise) and precise locations (m/z, RT, intensity) for all candidate compounds detected in the data [25].
Deep Learning Feature Detection Workflow
Advanced Methodologies
Sum of MRM (SMRM) for Large Biomolecule Quantification
Challenge: Large biomolecules (e.g., proteins, peptides) exist in multiple charged forms in ESI, distributing the total analyte signal across several ion peaks. Selecting a single precursor ion for traditional Multiple Reaction Monitoring (MRM) reduces signal intensity and can compromise sensitivity [26].
Solution: The Sum of MRM (SMRM) approach sums the intensities of MRM transitions from multiple precursor charge states of the same molecule. This boosts the detection signal and expands the dynamic range while maintaining analytical specificity [26].
Experimental Protocol for SMRM:
- Infusion Analysis: Directly infuse the large molecule standard into the mass spectrometer to acquire a full scan mass spectrum [26].
- Identify Charge States: Identify the 3-5 most abundant precursor charge states from the mass spectrum [26].
- Select Product Ions: For each precursor charge state, select 1-3 of the most intense and specific product ions generated via Collision-Induced Dissociation (CID) [26].
- Method Setup: Program the LC-MS/MS method to include all selected precursor ion → product ion transitions for the target analyte.
- Data Processing: Sum the peak areas or heights of all these MRM transitions to generate a combined chromatographic peak for quantification [26].
Validated Method for Trimethylamine N-Oxide (TMAO) Quantification
The following table summarizes a validated LC-MS/MS method for the gut-derived metabolite TMAO, demonstrating key principles of a sensitive and specific assay [27].
| Method Component | Specification |
|---|---|
| Analyte | Trimethylamine N-Oxide (TMAO) |
| Matrix | Human Blood Plasma |
| Sample Prep | Simple protein precipitation with a non-deuterated internal standard [27]. |
| LC-MS System | Triple Quadrupole Mass Spectrometer |
| Quantification | Lower Limit of Quantification (LLOQ) of 0.25 µM [27]. |
| Validation | Per EMA/FDA guidelines; intra- and inter-assay precision and trueness within limits [27]. |
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item | Function & Importance |
|---|---|
| LC-MS Grade Solvents | High-purity solvents (water, acetonitrile, methanol) are essential to minimize chemical background noise and prevent ion suppression [24] [23]. |
| LC-MS Grade Additives | High-quality acids (e.g., formic acid) and buffers (e.g., ammonium acetate) free of polymeric contaminants are critical for stable ionization and consistent performance [24]. |
| Nitrile Gloves | Worn during all handling steps to prevent contamination of samples, solvents, and surfaces with keratins, lipids, and other biomolecules from the skin [24]. |
| High-Quality Consumables | Use vials, pipette tips, and solid-phase extraction (SPE) plates from reputable manufacturers to minimize leachables like plasticizers and polyethylene glycols (PEG) [23]. |
| Dedicated Glassware | Use solvent bottles dedicated to specific instruments and solvents. Avoid washing with detergent to prevent introducing residual surfactants [24]. |
Contamination Sources and Effects
Technical Support Center
Troubleshooting Guides & FAQs
Issue 1: High Background Fluorescence / Low Signal-to-Noise Ratio
Q1: What causes uniformly high background fluorescence across all my bead sets, including negative controls?
- A: This is a classic sign of non-specific binding or contamination. Common causes include:
- Insufficient Blocking: The blocking buffer is inadequate or the incubation time was too short, leaving reactive sites on the bead surface.
- Contaminated Buffers or Reagents: Bacterial or particulate contamination in assay buffers can bind dyes non-specifically.
- Improper Wash Steps: Incomplete washing leaves unbound fluorescent detection antibody in the solution.
- Carryover Contamination: Contamination from previous runs or from improperly cleaned labware.
- A: This is a classic sign of non-specific binding or contamination. Common causes include:
Q2: My signal-to-noise ratio is poor for a specific analyte, while others are fine. What should I investigate?
- A: This points to an issue specific to that analyte's immunocomplex.
- Antibody Cross-Reactivity: The capture or detection antibody for that analyte may be cross-reacting with another protein or component in the sample matrix.
- Matrix Interference: Components in the sample (e.g., lipids, heterophilic antibodies, biotin) are interfering with the specific binding for that analyte.
- Degraded Reagents: The specific capture beads or detection antibody for that analyte may have degraded or been compromised.
- A: This points to an issue specific to that analyte's immunocomplex.
Experimental Protocol: Systematic Decontamination and Optimization
Objective: To identify and eliminate the source of high background fluorescence.
| Step | Procedure | Purpose | Key Parameter |
|---|---|---|---|
| 1 | Buffer Screening | Prepare fresh assay buffer and blocking buffer from new stock solutions. Filter all buffers through a 0.22 µm filter. | Eliminates contamination from old or particulate-laden buffers. |
| 2 | Alternative Blocking | Test a different, more robust blocking agent (e.g., 1% BSA + 5% Normal Serum from the host species of the detection antibody). | Saturates non-specific binding sites more effectively. |
| 3 | Increased Wash Stringency | Increase the number of wash cycles from 3 to 5. Add a mild detergent (e.g., 0.05% Tween-20) to the wash buffer. | Removes loosely bound proteins and reduces non-specific interactions. |
| 4 | Sample Pre-Clearance | Pre-incubate the sample with plain magnetic beads (no antibody) or a commercial heterophilic blocking reagent. | Removes components that bind non-specifically to the bead matrix or assay antibodies. |
Issue 2: Low Signal Intensity / Poor Assay Sensitivity
Q3: My positive controls are showing very low signal, indicating low assay sensitivity. What are the primary culprits?
- A: This indicates a failure in the formation of the detection immunocomplex.
- Antibody Titer: The concentration of the detection antibody is too low.
- Reaction Kinetics: The incubation time for the sample or detection antibody is insufficient for optimal binding.
- Fluorophore Degradation: The fluorescent dye conjugated to the detection antibody has been degraded by exposure to light or repeated freeze-thaw cycles.
- Instrument Calibration: The flow-based detector (e.g., Luminex scanner) is out of calibration.
- A: This indicates a failure in the formation of the detection immunocomplex.
Q4: The signal is low only for my high-plex panel, but single-plex assays work well. Why?
- A: This suggests "bead-bead" interference or antibody cross-talk in a multiplexed setting.
- Antibody Cross-Linking: Antibodies from different bead sets may be interacting with each other, forming large aggregates that quench signal or are lost during washing.
- Spectral Overlap: In highly multiplexed panels, the fluorescence emission spectra of different dyes may overlap, requiring compensation that can diminish perceived signal.
- A: This suggests "bead-bead" interference or antibody cross-talk in a multiplexed setting.
Experimental Protocol: Signal Amplification and Verification
Objective: To diagnose and correct causes of low signal intensity.
| Step | Procedure | Purpose | Key Parameter |
|---|---|---|---|
| 1 | Antibody Titration | Perform a checkerboard titration of the detection antibody against a fixed concentration of the analyte to find the optimal concentration. | Identifies the ideal antibody concentration for maximum signal without increasing background. |
| 2 | Incubation Kinetics | Increase the incubation time for the sample and detection antibody steps (e.g., from 1 hour to 2 hours at room temperature). | Allows more time for the binding equilibrium to be reached. |
| 3 | Fluorophore Integrity Check | Run the detection antibody alone on the instrument to verify its fluorescence intensity has not dropped compared to a new aliquot. | Confirms the fluorescent conjugate is still viable. |
| 4 | Bead Count Verification | Ensure a sufficient number of beads (e.g., >50 per region) are being acquired for analysis. Low bead counts can lead to unreliable and apparently low signals. | Validates the fundamental input for the assay. |
Issue 3: Poor Reproducibility and High Inter-Assay Variability
Q5: My replicate samples within the same plate show high variability (%CV > 20%). What steps can I take?
- A: This is often related to inconsistent liquid handling or reagent preparation.
- Pipetting Error: Manual pipetting of small volumes is a major source of error.
- Incomplete Resuspension: Magnetic beads settle quickly. Inconsistent vortexing or mixing leads to uneven bead distribution across wells.
- Edge Effects: Evaporation in outer wells of the microplate during incubations can alter reagent concentrations.
- A: This is often related to inconsistent liquid handling or reagent preparation.
Q6: The same sample gives different results when run on different days. How can I stabilize my assay?
- A: This inter-assay variability points to environmental or reagent batch issues.
- Temperature Fluctuations: Assay performance is sensitive to room temperature changes.
- Reagent Aliquot Variability: Using new aliquots of critical reagents (especially detection antibody) that have different storage histories.
- Operator Technique: Differences in technique between users or by the same user over time.
- A: This inter-assay variability points to environmental or reagent batch issues.
Experimental Protocol: Standardization for Reproducibility
Objective: To minimize technical variability within and between experiments.
| Step | Procedure | Purpose | Key Parameter |
|---|---|---|---|
| 1 | Automate Liquid Handling | Use an automated microplate washer and a repeater pipette for adding reagents. | Minimizes human error in volume dispensing. |
| 2 | Standardize Bead Handling | Implement a fixed vortexing protocol (e.g., 30 seconds at medium speed) before each bead transfer. | Ensures a homogeneous bead suspension for every well. |
| 3 | Control for Evaporation | Use a plate sealer during all incubation steps and run samples in non-edge wells or randomize sample placement. | Prevents concentration changes due to evaporation. |
| 4 | Implement Rigorous QC | Include a standardized QC sample (e.g., a pool of known positives) in every assay run. Track its results over time using a Levey-Jennings chart. | Allows for monitoring of inter-assay performance and early detection of drift. |
Visualizations
Diagram 1: FCMIA Workflow
Diagram 2: FCMIA Signal Generation
Diagram 3: Contamination Troubleshooting Logic
The Scientist's Toolkit: Essential Research Reagent Solutions
| Reagent / Material | Function & Importance |
|---|---|
| MagPlex / Magnetic Microspheres | Polystyrene beads impregnated with a precise ratio of two fluorescent dyes, giving each bead set a unique spectral signature (region) for multiplexing. The magnetic core enables efficient washing. |
| Carboxylated Bead Surface | Allows for stable, covalent coupling of capture antibodies via carbodiimide chemistry (e.g., EDC/Sulfo-NHS), which is more resistant to displacement and contamination than passive adsorption. |
| Biotinylated Detection Antibodies | Bind specifically to the captured analyte. The biotin moiety provides a universal binding site for the final fluorescent reporter, enabling signal amplification. |
| Streptavidin-Phycoerythrin (SA-PE) | The fluorescent reporter. Streptavidin binds with extremely high affinity to biotin, while Phycoerythrin is a bright, naturally fluorescent protein that provides a strong signal. |
| Phosphonate Buffer (for coupling) | A clean, amine-free buffer used during the antibody-bead coupling step. Contaminating amines (e.g., from Tris buffer) would compete with the antibody and reduce coupling efficiency. |
| Assay Buffer / Blocking Buffer | Typically a protein-based buffer (e.g., containing BSA or serum) used to block non-specific binding sites on the beads and to dilute samples/reagents, preventing high background. |
| Magnetic Plate Washer | Provides consistent and efficient washing of beads in a 96-well microplate format, which is critical for removing unbound material and reducing background signal. |
Technical Support Center: Troubleshooting Guides and FAQs
This technical support center is designed for researchers working to address contamination problems in surface measurements. It provides targeted solutions for common and complex issues encountered during Lateral Flow Immunoassay (LFIA) development and optimization.
Frequently Asked Questions (FAQs)
Q1: My LFIA strip shows no control line. What could be the cause? A missing control line indicates an invalid test. Potential causes and solutions include:
- Insufficient Sample Volume: Ensure the absorbent pad has adequate capacity to wick the entire sample volume. Increasing the thickness or length of the absorbent pad can resolve backflow and ensure complete sample migration [28].
- Improper Conjugate Release: Check if the conjugate pad is overly hydrophobic or if the release kinetics are too slow. Pre-treatment of the conjugate pad with surfactants like Tween-20 (<0.05%) or blockers like BSA can improve release [28] [29].
- Inactive Reagents: Verify the functionality of the antibodies used in the control line. The control line typically uses an anti-species antibody to capture labeled antibodies from the conjugate pad. Ensure these reagents have not degraded [30].
Q2: I am observing high background noise on the nitrocellulose membrane. How can I reduce it? High background, or "matrix effect," is often due to non-specific binding.
- Optimize Blocking Agents: Pre-treat the sample pad with blockers such as BSA (1%), casein (0.1–0.5%), or gelatin (0.05–0.1%) to occupy non-specific binding sites on the membrane and pads [28].
- Adjust Surfactant Concentration: Incorporate surfactants like Tween-20 or Triton X-100 (<0.05%) into the sample pad treatment buffer to reduce hydrophobic interactions and improve sample flow [28] [29].
- Purify Biological Reagents: Ensure that your detection and capture antibodies are highly purified to minimize cross-reactivity and non-specific binding [28] [29].
Q3: The test line is too faint for reliable visual interpretation. How can I enhance the signal? A faint test line indicates low sensitivity.
- Optimize Antibody Concentration: The amount of capture antibody spotted on the test line is critical. While typical ranges are 50–500 ng per strip (3–4 mm width), fine-tuning this concentration is necessary. Too much antibody can cause a "hook effect," while too little yields a weak signal [28] [31].
- Check Conjugation Efficiency: The pH of the conjugation buffer must be optimized to ensure complete binding of detector antibodies to colloidal gold nanoparticles. Perform a salt aggregation test to find the pH where nanoparticles remain stable upon salt addition, indicating successful antibody coating [28].
- Review Membrane Characteristics: A membrane with a smaller pore size (e.g., 8-10 µm) increases the wicking time, allowing more time for the antigen-antibody interaction to occur, which can enhance the signal [28] [29].
Q4: My assay for a small molecule contaminant (e.g., a mycotoxin) shows a positive result as the absence of a line. How can I make the result more user-friendly? You are using a competitive format, which is standard for small molecules [29] [32].
- Alternative Competitive Format: Some competitive assays are designed so that the labeled conjugate only binds to the test line in the presence of the analyte. This creates a familiar "line for positive" result. This often requires designing the strip with the analyte (or an analog) immobilized on the test line to capture the labeled antibody only if the sample is negative [29].
- Adopt a SERS-based Readout: Transition from a visual readout to a Surface-Enhanced Raman Scattering (SERS) readout. A SERS-LFIA provides a quantitative, instrumental output that is less ambiguous than interpreting the absence of a line. The intensity of the SERS signal is inversely proportional to the analyte concentration [33] [34].
Troubleshooting Guide: Common LFIA Issues and Solutions
Table 1: A summary of common problems, their potential causes, and recommended corrective actions.
| Problem | Symptom | Potential Cause | Corrective Action |
|---|---|---|---|
| No Control Line | Control line fails to develop. | Insufficient sample volume; Inactive control line antibody; Conjugate not released. | Check absorbent pad capacity [28]; Validate antibody activity [30]; Optimize conjugate pad treatment [28]. |
| High Background | Entire membrane is discolored, reducing contrast. | Non-specific binding; Sample matrix interference. | Use blockers (BSA, casein) in sample pad [28]; Include surfactants in buffer [29]; Purify antibodies [29]. |
| Faint Test Line | Weak signal, poor sensitivity. | Low antibody affinity; Suboptimal conjugation; Fast flow rate. | Titrate capture antibody concentration [31]; Optimize conjugation pH [28]; Use membrane with smaller pore size [28]. |
| False Positive | Test line appears with negative sample. | Cross-reactivity from impure antibodies. | Use monoclonal antibodies with distinct epitopes; Epitope mapping for capture/detector antibodies [28]. |
| Slow Flow Rate | Sample migrates too slowly. | Membrane with too small pore size; High viscosity sample. | Select membrane with larger pore size or faster capillary flow time [31]; Dilute or pre-treat sample to reduce viscosity [29]. |
Detailed Experimental Protocols
Protocol 1: Systematic Optimization of LFIA Components
This protocol provides a methodology for selecting and optimizing the core physical components of an LFIA strip [31].
Optimize the Nitrocellulose Membrane:
- Objective: Select a membrane that provides the best compromise between flow rate and sensitivity.
- Method: Test different membranes (e.g., Whatman FF80HP, FF120HP, FF170HP) with varying capillary flow rates (e.g., 60-100 s/4cm, 90-150 s/4cm, 140-200 s/4cm). Spray a visible protein (e.g., BSA) onto each membrane and assess the line continuity and sharpness. Apply your sample-conjugate mixture and evaluate the test line intensity. Slower flow rates (higher wicking time) generally enhance sensitivity by allowing more interaction time [28] [31].
Optimize the Absorbent Pad:
- Objective: Ensure complete sample wicking and prevent backflow.
- Method: Assemble strips with the optimized membrane and different absorbent pads (e.g., Whatman CF5, CF6, CF7). Measure the time taken for the sample front to travel the entire strip length. Select the pad that allows complete and consistent flow without backflow [31].
Optimize the Conjugate Pad:
- Objective: Ensure efficient release of the labeled conjugate.
- Method: Test different conjugate pad materials (e.g., Fusion 5, Standard 17, Standard 14) on the assembled strip. Assess which pad provides the strongest test line signal with the lowest background, indicating good release kinetics and low non-specific binding [31].
Optimize the Sample Pad:
- Objective: Ensure uniform sample application and effective filtration.
- Method: Compare different sample pads (e.g., Whatman CF1, CF3) for their ability to draw the sample consistently into the strip and filter out particulates if using complex samples like whole blood [31].
Titrate Capture Antibody:
- Objective: Determine the optimal amount of antibody for the test line.
- Method: Immobilize different concentrations of the capture antibody (e.g., 0.5, 1, and 2 µg per strip) onto the optimized membrane. Run positive and negative samples. Select the lowest concentration that yields a strong positive signal with a clean background [31].
Protocol 2: Conjugation of Antibodies to Gold Nanoparticles (AuNPs)
This is a critical step for preparing the detector reagent [28].
- Prepare Colloidal Gold: Synthesize 20-40 nm colloidal gold nanoparticles using the trisodium citrate reduction method (Turkevich-Frens method). The size can be customized by altering the citrate concentration [28] [32].
- pH Optimization: Adjust the pH of the colloidal gold solution using 0.1-0.2 M K₂CO₃. The optimal pH is typically slightly above the isoelectric point of the antibody. Determine this by adding 2 M NaCl to gold-antibody mixtures at different pHs; the optimum is the highest pH that prevents aggregation (no color change from red to blue) [28].
- Conjugation: Add the purified antibody to the pH-adjusted colloidal gold solution under constant stirring. The typical antibody concentration ranges from 2 to 20 µg per mL of gold sol.
- Stabilization: After 15-30 minutes, add a stabilizing agent (e.g., 1% BSA) to block any remaining reactive surfaces on the nanoparticles.
- Purification: Centrifuge the conjugate to remove unbound antibodies and re-suspend in a storage buffer containing sucrose, BSA, and surfactants.
- Application: The final conjugate is dispensed onto the optimized conjugate pad and dried, ready for strip assembly [28].
LFIA Workflow and Signal Generation
The following diagram illustrates the key stages of an LFIA, from sample application to result interpretation, which is fundamental for troubleshooting.
Diagram 1: Lateral Flow Immunoassay Workflow.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential materials and their functions in LFIA development for contamination analysis.
| Item | Function in the Assay | Key Considerations |
|---|---|---|
| Nitrocellulose Membrane | The porous matrix where capture antibodies are immobilized and the test/control lines form [28] [29]. | Pore size (1-20 µm) dictates flow rate and sensitivity. Smaller pores increase interaction time [28]. |
| Colloidal Gold Nanoparticles | The most common visual label, conjugated to detector antibodies. Produces a red color upon accumulation [28] [32]. | 20-40 nm particles offer a good balance of color intensity and stability. Conjugation is pH-sensitive [28]. |
| Monoclonal Antibodies | Highly specific capture and detection reagents that bind to a single epitope on the target analyte [29] [30]. | Essential for specificity. For sandwich assays, ensure capture and detector antibodies bind distinct, non-competing epitopes [28]. |
| Blocking Agents (BSA, Casein) | Proteins used to block non-specific binding sites on the membrane and pads, reducing background noise [28] [29]. | Concentration must be optimized (e.g., BSA 1%, Casein 0.1-0.5%) to prevent signal suppression [28]. |
| Surfactants (Tween-20) | Added to buffers to modify surface tension, ensuring uniform sample flow and aiding conjugate release from the pad [28] [29]. | Used at low concentrations (<0.05%). Critical for controlling wicking rates and preventing non-specific binding [28]. |
Technical Support Center
Troubleshooting Guides
Troubleshooting USP Chapter <800> Implementation
Problem: Inconsistent Pressure Differentials in Containment Areas
- Symptom: Unable to maintain the required negative pressure of 0.01 to 0.03 inches of water column relative to adjacent areas [35].
- Potential Cause: Airflow imbalances, room door left open, or leaks in the ventilation system.
- Solution:
- Verify that all doors to the buffer room and ante-room are closed properly.
- Conduct a smoke test to visualize airflow and identify leaks.
- Rebalance the HVAC system to ensure proper air supply and exhaust.
- Check the integrity of room seals around pipes, conduits, and ceiling panels [35].
Problem: CSTD Leakage During Administration
- Symptom: Visible liquid or vapor escape when using a Closed-System Transfer Device (CSTD).
- Potential Cause: Incompatible components, improper connection technique, or a defective device.
- Solution:
- Confirm that all CSTD components are from the same manufacturer and are designed to work together.
- Retrain personnel on the correct technique for making and breaking connections.
- Perform a pressure decay test or similar validation check on the CSTD before use.
- Replace any device that fails validation or shows signs of damage [35].
Troubleshooting SEMI Protocol Implementation
Problem: Intermittent SECS/GEM Communication Failure
- Symptom: Host system randomly loses connection to the manufacturing equipment.
- Potential Cause: Man-in-the-Middle (MITM) attack sending a "separate" request, network instability, or incorrect HSMS (High-Speed SECS Message Services) parameters.
- Solution:
- Inspect network architecture for unauthorized devices and implement strict access control lists (ACLs).
- Use a network monitoring tool to detect anomalous "separate" requests.
- Verify and match the HSMS communication parameters (e.g., T3, T5, T6, T7 timeouts) between the host and equipment [36].
- Utilize solutions that provide continuous traffic monitoring and anomaly detection [36].
Problem: SECS/GEM Interface Becomes Unresponsive
- Symptom: Equipment data collection stops; the interface does not respond to commands.
- Potential Cause: Denial-of-Service (DoS) attack from a high volume of messages, or a system resource leak in the interface software.
- Solution:
- Deploy an Intrusion Prevention System (IPS) with rate-limiting capabilities to filter excessive SECS/GEM traffic.
- Restart the interface service or application to clear resource leaks.
- Analyze communication logs to identify the source of the message flood.
- Implement granular security controls to filter commands based on operational context [36].
Frequently Asked Questions (FAQs)
Q1: What is the core purpose of USP Chapter <800>? A1: USP <800> provides standards for the safe handling of hazardous drugs (HDs) to protect healthcare personnel, patients, and the environment from exposure risks. It covers the entire lifecycle of an HD, from receipt and storage to preparation, administration, and waste disposal [37] [35].
Q2: Which drugs are considered "hazardous" under USP <800>? A2: A drug is considered hazardous if it exhibits one or more of these characteristics: carcinogenicity, teratogenicity or developmental toxicity, reproductive toxicity, organ toxicity at low doses, genotoxicity, or has a structure and toxicity profile similar to existing hazardous drugs. The primary reference list is the NIOSH List of Hazardous Drugs in Healthcare Settings [37].
Q3: What are the key facility requirements for compounding hazardous drugs under USP <800>? A3: Key requirements include:
- Using a containment primary engineering control (C-PEC) like a ventilated cabinet.
- Placing the C-PEC in a containment secondary engineering control (C-SEC) room with negative pressure (0.01 to 0.03 inch WC).
- Ensuring the room has a minimum of 12 air changes per hour.
- Venting the C-PEC directly to the outside [35].
Q4: What are SECS/GEM protocols, and why are they important? A4: SECS/GEM is a set of communication standards maintained by SEMI that enables standardized communication between semiconductor manufacturing equipment and factory host systems. This allows for equipment automation, data collection for monitoring and analysis, and is a foundational element for Industry 4.0 in semiconductor manufacturing [38] [36].
Q5: What are the primary cybersecurity risks associated with SECS/GEM? A5: The protocol lacks built-in security features, making it vulnerable to:
- Man-in-the-Middle (MITM) Attacks: An attacker can disrupt communication by disconnecting the legitimate host [36].
- Denial-of-Service (DoS) Attacks: Flooding the interface with messages can crash it [36].
- Malicious File Exploitation: Tampered SML files can cause system crashes or loss of control [36].
Q6: How can SECS/GEM cybersecurity be improved? A6: Recommended measures include:
- Implementing strict network access control and segmentation.
- Deploying OT-specific IPS solutions for traffic monitoring and rate limiting.
- Using malware detection and advanced threat detection systems.
- Regularly monitoring and maintaining comprehensive visibility of network traffic [36].
Table 1: Key USP Chapter <800> Facility and Environmental Control Requirements
| Parameter | Requirement | Note / Rationale |
|---|---|---|
| Pressure Differential | 0.01 to 0.03 inch WC (negative) | Relative to adjacent areas; prevents contamination escape [35]. |
| Air Changes Per Hour (ACPH) | Minimum of 12 | Ensures sufficient air exchange in the compounding room [35]. |
| C-PEC Venting | Vented directly to the outside | Prevents recirculation of hazardous drug vapors indoors [35]. |
| CSTD Use | Required for administration | Minimizes exposure to nurses administering antineoplastic HDs [35]. |
Table 2: Common SEMI Standards for Communication and Control
| Standard Number | Name | Primary Function |
|---|---|---|
| SEMI E4 | SECS-I | Defines the RS-232-based physical layer for SECS/GEM communication [36]. |
| SEMI E5 | SECS-II | Defines the message content and structure for SECS/GEM [38] [36]. |
| SEMI E37 | HSMS | Defines the TCP/IP-based communication for SECS/GEM, replacing E4 in modern fabs [36]. |
| SEMI E30 | GEM | Defines a generic model for state models and common equipment behavior for automation [38]. |
| SEMI E134 | Data Collection Management | Specifies how factory hosts can configure and manage data collection from equipment [38]. |
Experimental Protocols for Contamination Control
Protocol 1: Surface Wipe Sampling for Hazardous Drug Residue
- Objective: To detect and quantify surface contamination by hazardous drugs in compounding and administration areas.
- Materials:
- Pre-moistened specialized wipes (e.g., gauze with a sampling solution)
- Sampling template (e.g., 10cm x 10cm)
- Sample collection vials
- Cold chain shipping container
- LC-MS/MS (Liquid Chromatography with Tandem Mass Spectrometry) analytical service
- Methodology:
- Don appropriate personal protective equipment (PPE).
- Place the sampling template on the surface to be tested (e.g., workbench, countertop, door handle).
- Use a pre-moistened wipe to thoroughly wipe the area within the template, using a consistent pattern.
- Place the used wipe into a labeled sample collection vial and seal it.
- Repeat steps for all sampled surfaces and include a field blank (a wipe that is opened but not used).
- Store and ship all samples in a cold chain container to the analytical lab.
- Analyze results against established action levels to assess decontamination effectiveness [35] [39].
Protocol 2: Network Traffic Analysis for SECS/GEM Anomaly Detection
- Objective: To identify potential cyber-intrusions or malfunctions in the semiconductor equipment communication network that could impact process integrity.
- Materials:
- Network TAP (Test Access Point) or SPAN (Switched Port Analyzer) port
- OT-network monitoring appliance (e.g., one capable of deep packet inspection)
- Security Information and Event Management (SIEM) system or log aggregator
- Methodology:
- Deploy a network TAP or configure a SPAN port on the switch connecting the SECS/GEM equipment to the factory network.
- Direct a copy of all network traffic to the OT-monitoring appliance.
- Configure the appliance to decode HSMS/SECS-II traffic and establish a baseline of normal communication patterns (e.g., typical message types, volumes, and source-destination pairs).
- Set alerts for anomalies such as:
- A high rate of "separate" requests.
- SECS/GEM messages originating from unauthorized IP addresses.
- An unusually high volume of messages from a single source in a short time (potential DoS).
- Correlate alerts with other system logs in the SIEM to investigate potential security incidents [36].
Research Reagent Solutions and Essential Materials
Table 3: Key Materials for Contamination Control and Surface Measurement Research
| Item | Function |
|---|---|
| Closed-System Transfer Device (CSTD) | A drug transfer device that mechanically prohibits the transfer of environmental contaminants into the system and the escape of hazardous drug or vapor concentrations outside the system [35]. |
| Containment Primary Engineering Control (C-PEC) | A ventilated device (e.g., Biological Safety Cabinet, Compounding Aseptic Containment Isolator) designed to provide worker and product protection during HD preparation [35]. |
| Specialized Wipe Samplers | Pre-prepared wipes with a defined material and solution for standardized surface sampling of chemical residues. |
| LC-MS/MS Analytical Services | Highly sensitive analytical testing used to detect and quantify trace levels of hazardous drugs on surfaces. |
| OT-Native Network Security Appliance | A hardware or software solution designed to monitor and control operational technology network traffic, providing visibility and protection for protocols like SECS/GEM [36]. |
Workflow and Relationship Diagrams
USP <800> HD Handling Workflow
SECS/GEM Cybersecurity Risks & Defenses
FAQs: Core Principles of Wipe Sampling
Q1: What is the primary purpose of wipe sampling for antineoplastic drugs (ADs) in research settings?
Wipe sampling is the established methodology for determining the level of hazardous drug residue on surfaces in workplaces such as pharmacies and patient care areas [40]. Its primary purposes within a research context are to:
- Characterize Potential Dermal Exposure: Dermal uptake is considered the most likely route of occupational exposure for low-molecular-weight antineoplastic drugs. Wipe sampling evaluates contamination on surfaces that may lead to dermal absorption by researchers and healthcare workers [40].
- Evaluate Control Measures: It is used to assess the effectiveness of engineering controls (e.g., ventilated enclosures), work practices, personal protective equipment (PPE), and cleaning procedures [40] [41].
- Establish Baselines and Monitor Trends: Sampling is performed initially to establish a baseline of contamination and then routinely (e.g., every six months as suggested by USP <800>) to verify containment and track trends over time [42] [43].
Q2: Which surfaces are most critical to sample for antineoplastic drug contamination?
Research has identified that contamination is not uniform and is often found on high-touch surfaces. The most commonly contaminated locations include [44] [43]:
- Interiors of Compounding Primary Engineering Controls (C-PECs) such as biological safety cabinets.
- Nursing counters and surfaces in staging areas.
- Patient administration areas, including IV poles/pumps and armchairs.
- Floors directly under the C-PEC or in adjacent areas.
- Doorknobs/handles, Hazardous Drug (HD) waste containers, and storage shelves.
Q3: What are the key challenges associated with interpreting wipe sample results?
One of the biggest problems is the difficulty in interpreting results due to a lack of standardization and several variables [45] [46] [41].
- No Standardized Hygienic Guidance Values (HGVs): For most drugs, there are no universally accepted surface contamination action limits. While any detectable amount should be addressed, it is challenging to benchmark the risk [46] [43] [47].
- Variable Sampling Efficiency: The recovery efficiency of a wipe can be affected by the surface material (smooth vs. rough), the type of wipe, the solvent used, and the operator's technique. This makes it difficult to compare results from different studies or even different surfaces within the same study [45] [41].
- Result Reporting: Results are typically reported as a mass of analyte collected (e.g., nanograms). Converting this to a concentration (e.g., ng/cm²) requires a standardized sampling area, and even then, the efficiency of the wipe itself is often not accounted for [45].
Experimental Protocols: Standardized Wipe Sampling Methodology
The following protocol provides a detailed methodology for the collection of surface wipe samples for the analysis of antineoplastic drug residues, based on established procedures in the literature [40] [41] [48].
Materials and Reagents
| Item | Specification/Function |
|---|---|
| Wipe Material | Commercially available filter paper, gauze, or specialized sampling swabs (e.g., Whatman filter paper, polyester swabs). The material should be low in analytes of interest. |
| Solvent | A suitable solvent for the target analytes, such as a mixture of water with a mild surfactant (e.g., 0.03% sodium dodecyl sulfate) or methanol. The choice depends on the drug's solubility [46] [40]. |
| Sampling Template | A sterile, disposable template (e.g., 10 cm x 10 cm = 100 cm²) to delineate the sampling area consistently [40] [41]. |
| Sample Containers | Pre-cleaned, labeled containers (e.g., glass or plastic vials) that are chemically compatible with the sample and solvent. |
| Personal Protective Equipment (PPE) | Single-use nitrile gloves, lab coat, and safety glasses to prevent sample contamination and analyst exposure. |
| Cooler & Cold Packs | For transporting samples at a stable, cool temperature if required. |
Step-by-Step Collection Procedure
Planning and Documentation:
- Identify the sampling locations based on a risk assessment of the workflow, from drug receipt to administration and waste disposal [48].
- Document the sampling plan, including the date, time, specific location description, target analytes, and surface type. Photographing or sketching the sampling areas is highly recommended [41].
Sample Collection:
- Don clean PPE.
- Place the sampling template on the pre-identified surface.
- Moisten the wipe with the chosen solvent. Avoid over-saturation.
- Wipe the entire area within the template using a consistent pattern (e.g., an "S" pattern). Apply firm, consistent pressure.
- Fold the wipe with the exposed side inward.
- Wipe the same area again in a perpendicular direction to maximize recovery. Some protocols use a second, dry wipe for the same area [40].
- Carefully place the wipe(s) into the sample container and seal it tightly to prevent evaporation or leakage.
Post-Collection Handling:
- Label the container clearly with a unique sample ID.
- Place samples in a cooler with cold packs (if required for stability) for transport to the laboratory.
- Maintain a chain of custody form to track sample handling from collection to analysis.
Workflow Diagram
The following diagram illustrates the complete wipe sampling process from planning to corrective action.
Troubleshooting Guides: Common Experimental Issues
Problem: Low or Inconsistent Analytic Recovery During Method Validation
- Potential Cause 1: Inefficient desorption of the analyte from the wipe material.
- Solution: Optimize the desorption solvent composition, volume, and shaking time/agitation speed during the extraction step. A mixture of solvents may be required for certain drugs [46].
- Potential Cause 2: The wipe material or solvent is not optimal for the target drug.
- Potential Cause 3: Analytic degradation during storage.
- Solution: Conduct stability studies to establish maximum holding times. Store samples at recommended temperatures (often frozen), and protect from light. For volatile compounds, analysis should be performed quickly, as holding times may be as short as 48 hours for some methods [45].
Problem: High Background Interference or Contamination in Blanks
- Potential Cause 1: Contamination from the sampling kit components (wipes, containers, solvents).
- Solution: Always include field blanks and trip blanks in the sample batch. Use high-purity solvents and ensure all components are certified clean for the analytes of interest [48].
- Potential Cause 2: Cross-contamination during sample collection.
- Solution: Change gloves between each sample collection. Use a new, sterile template for each sample or decontaminate it thoroughly between uses [41].
Problem: High Variability Between Replicate Samples
- Potential Cause 1: Inconsistent sampling technique (e.g., varying pressure, pattern, or solvent volume).
- Potential Cause 2: Inhomogeneous distribution of contamination on the surface.
- Solution: This is a inherent challenge. Increase the number of replicate samples or consider composite sampling from a larger area to get a more representative result [45].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and their functions for wipe sampling experiments.
Table: Essential Materials for Wipe Sampling of Antineoplastic Drugs
| Item | Function & Importance |
|---|---|
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | The current gold-standard analytical method for most antineoplastic drugs. It provides high sensitivity (detection in pg/cm²), specificity, and the ability to quantify multiple drugs simultaneously (multiplexing) [44] [40]. |
| Inductively Coupled Plasma Mass Spectrometry (ICP-MS) | The preferred method for detecting elements like platinum from platinum-based antineoplastic drugs (e.g., cisplatin). It is highly sensitive and specific for metallic elements [47]. |
| Standardized Sampling Templates | Creates a consistent and known surface area (typically 100 cm²) for sampling, which is crucial for converting the mass of drug found into a surface concentration (e.g., ng/cm²) [44] [41]. |
| High-Purity Solvents (e.g., Methanol, Water with Surfactant) | Used to wet the wipe, enhancing the adsorption and removal of drug residues from the surface. The solvent must be compatible with both the drug and the subsequent analytical method [46] [40]. |
| Closed System Transfer Devices (CSTDs) | Although not a sampling reagent, CSTDs are a critical engineering control. Studies show that institutions using CSTDs have significantly lower surface contamination, making them a key solution for mitigating the contamination problem being studied [44] [41]. |
Data Presentation: Analytical Method Comparison
The selection of an analytical method is a critical step in experimental design. The table below summarizes the key characteristics of the primary techniques used.
Table: Comparison of Analytical Methods for Wipe Sample Analysis
| Method | Typical Analytes | Key Advantages | Key Limitations |
|---|---|---|---|
| LC-MS/MS & GC-MS/MS [44] [40] | Cyclophosphamide, methotrexate, 5-fluorouracil, etc. | High sensitivity and specificity; Can detect multiple drugs simultaneously; Considered the gold standard. | High equipment cost; Requires trained personnel; Lengthy turnaround time; High per-sample cost. |
| ICP-MS [47] | Platinum-based drugs (Cisplatin, Carboplatin). | Exceptional sensitivity for specific elements; User-friendly methods can be developed. | Only detects specific elements, not the whole drug molecule; Cannot distinguish between different platinum-containing drugs without speciation. |
| Immunoassay Techniques (e.g., FCMIA, LFIA) [40] | Specific targeted drugs (scope is currently limited). | Potential for rapid, on-site analysis; Lower cost; Shorter response time. | Limited multiplexing capability; Currently not widely available for a broad range of ADs; May have cross-reactivity issues. |
Strategies for Effective Decontamination and Exposure Control
Surface contamination monitoring is a vital element of effective exposure assessment and control programs across various scientific and industrial fields, from hazardous drug compounding in research laboratories to environmental and water quality management [49] [50]. A well-designed monitoring program serves as an essential tool for validating the effectiveness of preventive controls, engineering solutions, and safety protocols [51]. Within the broader context of contamination research, establishing a robust monitoring framework enables researchers and professionals to move from reactive problem-solving to proactive risk management. This technical support guide addresses the key components of developing such a program, focusing on the critical decisions surrounding monitoring frequency, strategic location selection, and establishing performance benchmarks that together form the foundation of a data-driven contamination control strategy.
Core Components of a Surface Monitoring Program
Frequently Asked Questions (FAQs)
Q1: What is the primary goal of a surface monitoring program? The primary goal is to find pathogens, hazardous chemicals, or allergens in the environment before they contaminate your product or process. Secondary goals include assessing the effectiveness of cleaning, sanitation, and employee hygiene practices [51].
Q2: How do I determine where to collect surface samples? Sampling locations should be chosen based on a risk assessment that identifies areas with the greatest risk of contamination to your product or process. Key locations include critical surfaces (where product/process is exposed), critical control points (where contamination transfer is controlled), and sources with high dispersion rates [52]. The "Zone Concept" provides a systematic framework for this selection [51].
Q3: What is an appropriate sampling frequency for my program? Sampling frequency is not one-size-fits-all and should be based on your process risk, historical data, and the specific zone being monitored. For high-risk Zone 1 areas, daily or weekly sampling may be necessary, while lower-risk zones may require only weekly, monthly, or quarterly monitoring [51]. Frequency should increase following adverse events or process changes [51].
Q4: How should I interpret surface contamination results? Without universally established contamination limits, results must often be interpreted on a case-by-case or site-specific basis [49]. Establish objective cleanliness criteria based on factors such as toxicity, natural background levels, environmental target levels, and the detection capabilities of your analytical methods [49].
Q5: What should I do when contamination is detected? A predefined action plan should include immediate surface decontamination, followed by resampling to verify effectiveness [53]. For persistent contamination, conduct a root cause analysis to identify the source and implement corrective and preventive actions (CAPA), which may include reviewing engineering controls, work practices, and cleaning procedures [53] [50].
Troubleshooting Common Monitoring Challenges
Problem: Inconsistent or misleading monitoring results.
- Potential Cause: Inadequate sampling technique leading to cross-contamination or insufficient sample collection.
- Solution: Standardize aseptic collection methods. Use pre-sterilized tools with appropriate transport buffers that neutralize common sanitizers. Train personnel on proper technique to avoid contaminating specimens [51].
Problem: Failing to detect contamination events.
- Potential Cause: Sampling frequency is too low to capture transient contamination peaks.
- Solution: For processes with known short-term dynamics (e.g., after specific events like precipitation in water systems or batch processing in labs), implement a targeted, event-driven sampling strategy rather than simply increasing routine frequency [54]. One study on water monitoring found that at least bi-weekly sampling was needed to detect precipitation events with >90% probability, but a more efficient approach used three targeted samples triggered by precipitation measurements [54].
Problem: Unable to determine if contamination level is acceptable.
- Potential Cause: Lack of established, site-specific action levels or benchmarks.
- Solution: Develop internal action and alert levels based on statistical analysis of your historical monitoring data. For a cleanroom with normally distributed data, one method sets the action level at three standard deviations above the mean and the alert level at two standard deviations above the mean [52].
Problem: High costs associated with frequent monitoring and laboratory analysis.
- Potential Cause: Reliance solely on off-site laboratory analysis, which is time-consuming and costly.
- Solution: Integrate rapid, on-site testing technologies where available. For example, lateral flow immunoassays (LFIAs) can provide results for hazardous drugs in less than 10 minutes, saving considerable time and money compared to conventional wipe sampling with off-site analysis [55]. This allows for more frequent monitoring and immediate corrective action.
Strategic Location Selection: The Zone Concept
The "Zone Concept" provides a systematic, risk-based framework for organizing your environmental sampling program, prioritizing areas based on their proximity to the product or process and the associated risk of contamination [51].
Table: The Four-Zone Framework for Environmental Monitoring
| Zone | Description | Example Locations | Recommended Tests |
|---|---|---|---|
| Zone 1 | Direct product contact surfaces | Conveyor belts, filler needles, utensils, gloves | Indicator bacteria (APC, coliforms), specific allergens; pathogen testing requires careful consideration due to potential regulatory implications [51]. |
| Zone 2 | Non-product contact surfaces in close proximity to Zone 1 | Equipment frames, control panels, drip shields | Salmonella and/or L. monocytogenes, indicator bacteria (e.g., Listeria spp., APC, coliforms) [51]. |
| Zone 3 | Non-product contact surfaces in the open processing area, further from Zone 1 | Floors, walls, drains, cleaning equipment, carts | Salmonella and/or L. monocytogenes, indicator bacteria (e.g., Listeria spp., APC, coliforms) [51]. |
| Zone 4 | Support areas outside the open processing area | Locker rooms, cafeterias, hallways, warehouses | Salmonella and/or L. monocytogenes, indicator bacteria; frequency is typically lower [51]. |
The following workflow illustrates the process of designing a monitoring plan based on the Zone Concept and risk assessment:
Determining Sampling Frequency and Establishing Benchmarks
Sampling Frequency Guidance
Sampling frequency should be dynamic and adapt to risk, historical data, and process changes [51]. The table below provides a general framework, which should be tailored to your specific operation.
Table: Framework for Determining Sampling Frequency
| Factor Influencing Frequency | Recommended Action | Application Example |
|---|---|---|
| Program Stage | Begin with frequent sampling and large surface areas to establish a baseline and identify problem areas. Frequency can be optimized once sufficient data is collected and controls are validated [51]. | When starting a new program, sample numerous sites weekly. After establishing control, rotate sites to cover all potential locations monthly [51]. |
| Zone Risk Level | Align frequency with zone risk: Zone 1 (most frequent) to Zone 4 (least frequent) [51]. | Zone 1: Daily/Weekly; Zone 2 & 3: Weekly; Zone 4: Monthly/Quarterly [51]. |
| Historical Results & Trends | Increase frequency following an adverse result or if trends indicate loss of control. Reduce frequency only when data confirms a stable, controlled state over an extended period [51]. | Double the sampling frequency in an area where a positive result was found until consecutive negative results are achieved. |
| Process or Event Changes | Increase frequency following any event that increases contamination risk [51]. | After construction, equipment installation, a pest intrusion, or a major spill [51]. |
| Parameter Dynamics | For parameters with rapid fluctuations, use high-frequency in-situ sensors or event-driven sampling to capture peak concentrations that would be missed by grab sampling [56] [54]. | In water quality, use in-situ sondes to capture transient events. For karstic springs, trigger sampling by precipitation measurements [54]. |
Setting Action and Alert Levels
Establishing statistical benchmarks for your data is crucial for objective interpretation. Action and alert levels are key tools for this.
- Action Level: The concentration of contaminants that should not be exceeded, prompting immediate corrective action if breached [52].
- Alert Level: An airborne or surface concentration that is greater than normally found, serving as an early warning of potentially unacceptable conditions [52].
For a cleanroom or process with roughly normally distributed data, you can set levels statistically [52]:
- Option 1: Set the action level at the regulatory limit (if one exists) and the alert level at two standard deviations (95% confidence) above the mean.
- Option 2: Set the action level at three standard deviations (99.7% confidence) above the mean (a value that should rarely be exceeded), and the alert level at two standard deviations above the mean.
For non-normally distributed data, control levels can be set using percentiles [52]:
- The 95th percentile is equivalent to the 95% confidence limit.
- The 99.7th percentile is equivalent to the 99.7% confidence limit.
Experimental Protocols and Methodologies
Standard Wipe Sampling Procedure for Surface Contamination
This protocol is adapted from standard methods used for monitoring hazardous drug [53] [50] and chemical [49] surface contamination.
- Preparation: Select the appropriate sampling tool (e.g., sterile sponge in bag, swab) with a neutralizing transport buffer to inactivate common sanitizers [51].
- Define Sampling Area: Use a defined surface area template (e.g., 10x10 cm) for consistent quantitative results [55].
- Aseptic Collection: Don sterile gloves. Wipe the defined area systematically, applying firm pressure. For large surfaces, use an overlapping "S" pattern; for small or irregular surfaces, ensure the entire swab/sponge head is used to cover the area.
- Sample Recovery: Carefully place the sponge or swab back into its transport container with the neutralizing buffer, ensuring the collected material is immersed.
- Labeling and Chain of Custody: Label the sample container with a unique ID, date, time, and location. Complete the chain of custody form and maintain detailed records in a sampling site log [51].
- Storage and Transport: Store samples chilled and transport to the laboratory ideally within 24 hours to preserve sample integrity [51].
Protocol for a Hazardous Drug Contamination Study
A 2025 study evaluating a hazardous drug surveillance program provides a model for a systematic monitoring experiment [53].
- Objective: To evaluate the impact of a wipe sampling technology and new environmental procedures on identifying and reducing hazardous drug (HD) surface contamination [53].
- Study Design: A 16-week longitudinal evaluation.
- Sampling Sites: 25 sites within a cleanroom suite and infusion areas, selected through a risk stratification assessment (categorized as high, medium, or low-risk) [53].
- Parameters Monitored: Surface wipe samples were tested for methotrexate, doxorubicin, and cyclophosphamide using a rapid immunoassay system [53].
- Methodology:
- Baseline Sampling: Initial wipe sampling was performed to establish a benchmark contamination level.
- Intervention: Standard Operating Procedures (SOPs) for testing, decontamination, and retesting were implemented.
- Routine Monitoring: Sampling was conducted periodically (e.g., every six months or as needed) in accordance with the risk-based plan [55].
- Corrective Action: For any positive result, decontamination was performed immediately, followed by resampling to verify effectiveness. Persistent positives underwent a formal Corrective and Preventive Action (CAPA) analysis [53].
- Outcome Measures: The number and percentage of positive samples before and after decontamination were tracked to measure the program's success [53].
The Scientist's Toolkit: Key Research Reagent Solutions
Table: Essential Materials for Surface Contamination Monitoring
| Item | Function | Application Notes |
|---|---|---|
| Sterile Sponges/Swabs | To physically remove microorganisms or chemical residues from a defined surface area. | Pre-moistened with a neutralizing buffer. Sponges are ideal for large, flat surfaces; swabs are better for small or irregular surfaces [51]. |
| Neutralizing Transport Buffers | To preserve the sample during transport and neutralize residual sanitizers (e.g., quaternary ammonium compounds, chlorine, phenolics) that could kill collected microbes or degrade chemicals. | Common types include D/E broth, Letheen broth, and Neutralizing Buffer. Selection should be based on the sanitizers used in the facility [51]. |
| Lateral Flow Immunoassay (LFIA) Kits | For rapid, on-site detection of specific hazardous compounds (e.g., methotrexate, doxorubicin). | Provides qualitative (positive/negative) results in minutes, enabling immediate corrective action. Cheaper and faster than off-site lab analysis [55]. |
| Adenosine Triphosphate (ATP) Meters | To measure overall surface cleanliness by detecting biological residue through a bioluminescent reaction. | Provides immediate results but is non-specific. Useful for routine verification of cleaning effectiveness, though it should be validated against specific contaminant tests [51]. |
| Surface Area Template | To standardize the surface area being sampled, allowing results to be reported quantitatively (e.g., ng/cm²). | Typically a sterile, disposable stencil defining a specific area (e.g., 100 cm²) [55]. |
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Our autoclave cycle completes, but biological indicators show that sterilization is not being achieved. What could be wrong? The failure to achieve sterility is often due to air entrapment preventing steam contact. Ensure the autoclave drain screen is clean and not blocked by debris, as this can create an air layer at the bottom, preventing efficient operation [57]. Also, verify that materials are packed to allow steam penetration and that the autoclave is routinely maintained and validated with biological indicators (e.g., Geobacillus stearothermophilus spore strips) [58] [57]. A sterility assurance level of less than one in a million (10⁻⁶) must be the target [58].
Q2: How do I determine whether a surface requires disinfection or sterilization? The required level of decontamination is based on the intended use of the item and the risk of pathogen transmission [57]. Critical items that enter sterile tissue require sterilization. Non-critical environmental surfaces (e.g., floors, lab benches) typically require low- or intermediate-level disinfection, while contaminated lab surfaces may require high-level disinfection [57]. The risk is a function of the probability of contamination, patient vulnerability, and potential for exposure (e.g., high-touch vs. low-touch surfaces) [17].
Q3: What is the proper sequence for cleaning and disinfecting a laboratory room? Always proceed in a systematic manner:
- From cleaner to dirtier areas to avoid spreading contamination (e.g., clean low-touch surfaces before high-touch surfaces) [17].
- From high to low (top to bottom) to prevent dirt and microorganisms from falling onto cleaned areas [17].
- In a terminal clean, start with shared equipment, then proceed to surfaces outside the patient zone, and finally to surfaces inside the patient zone [17].
Q4: How can we verify that our decontamination procedures for equipment are effective? Surface contamination sampling is a vital element for verifying effectiveness [49]. Techniques include:
- Standard wipe sampling: A surface is wiped with a dry or wetted filter, which is then analyzed in a lab [49].
- Direct-reading media: Using pH sticks or colorimetric pads for instant results [49].
- Immunoassay test kits: Provide quantitative on-site analysis for specific contaminants [49]. Results should be interpreted against site-specific cleanliness criteria [49].
Troubleshooting Common Decontamination Issues
The table below outlines specific problems, their potential causes, and recommended solutions.
| Problem | Potential Root Cause | Recommended Solution |
|---|---|---|
| Ineffective Surface Disinfection | Incorrect disinfectant choice for target pathogen; organic matter present; insufficient contact time [58] [57]. | Select an appropriate-level disinfectant (check for tuberculocidal claim for intermediate level); pre-clean surface to remove soil; ensure surface remains wet for the manufacturer's recommended contact time [58] [57]. |
| Liquid Waste Decontamination Failure | Incorrect chemical concentration; insufficient contact time; high bioburden [58]. | Validate decontamination procedure for specific agent and material; use chemical disinfectants per manufacturer specs, ensuring correct concentration and hold time; for large volumes, use an Effluent Decontamination System (EDS) [58]. |
| Permeation of Chemical Contaminants through PPE | Inappropriate glove or suit material for the chemical; exceeding the breakthrough time [49]. | Sample the inner surface of PPE to test for adequacy; select PPE material resistant to the specific chemicals handled; establish and adhere to safe work durations [49]. |
| Migration of Contaminants into Clean Areas | Inadequate decontamination procedures for items or personnel leaving the hot zone; improper work zone boundaries [49]. | Incorporate surface contamination sampling at zone boundaries to monitor for migration; modify decontamination procedures and zone boundaries based on findings [49]. |
Experimental Protocols for Key Procedures
Protocol 1: Validating an Autoclave Cycle Using Biological Indicators
- Objective: To confirm the autoclave achieves a sterility assurance level of 10⁻⁶.
- Methodology:
- Place biological indicator strips containing Geobacillus stearothermophilus spores (known for high heat resistance) into the geometric center of a mock load, typically the coldest point [57].
- Run a standard autoclave cycle (e.g., 121°C for at least 30 minutes for a 1-liter load) [58].
- Aseptically transfer the processed spore strip to a growth medium and incubate according to the manufacturer's specifications (e.g., 55-60°C for 24-48 hours).
- Simultaneously, run an untreated control strip to confirm spore viability.
- Interpretation: No growth in the processed sample indicates a successful cycle. Growth indicates failure, and the autoclave must be serviced, and the load re-processed [58] [57].
Protocol 2: Standard Wipe Sampling for Surface Contamination
- Objective: To quantitatively evaluate the level of chemical or microbial contamination on a surface after decontamination.
- Methodology [49]:
- Mark a standard area (e.g., 10x10 cm) using a sterile template.
- Don clean gloves. Moisten a sterile sampling filter with a suitable solution (e.g., deionized water for salts, a mild surfactant for organics).
- Wipe the entire defined area systematically, applying moderate pressure. First, wipe horizontally across the surface, then fold the cloth to a clean side and wipe vertically.
- Place the used filter into a clean, labeled container.
- Submit the sample to a laboratory for analysis (e.g., chemical analysis, microbial culture).
- Interpretation: Compare results against pre-established, site-specific criteria for surface cleanliness, which may be based on toxicity, background levels, or remediation targets [49].
Workflow and Relationship Diagrams
Decontamination Method Selection Logic
Terminal Cleaning Workflow for a Contained Space
The Scientist's Toolkit: Research Reagent Solutions
The table below details key materials and their functions in decontamination and contamination assessment procedures.
| Research Reagent / Material | Primary Function in Decontamination |
|---|---|
| Biological Indicators (BIs) | Strips or vials containing bacterial spores (e.g., G. stearothermophilus for steam, B. atrophaeus for VHP/ETO). Used to validate sterilization cycles by challenging the process with a known, highly resistant microorganism [58] [57]. |
| Chemical Indicators | Autoclave tape or integrators that change color when exposed to specific sterilization parameters (e.g., heat, steam). Provide an immediate, visual indication that an item has been processed but do not prove sterility [57]. |
| High-Level Disinfectants | Concentrated chemical germicides (e.g., hydrogen peroxide, peracetic acid, concentrated bleach). Used to kill all microorganisms except high numbers of bacterial spores, typically with short contact times (10-30 mins) [57]. |
| Intermediate-Level Disinfectants | EPA-approved "hospital disinfectants" that are tuberculocidal (e.g., certain phenolics, iodophors). Kill vegetative bacteria, including M. tuberculosis, all fungi, and inactivate most viruses. Suitable for lab benches and non-critical equipment [57] [17]. |
| Immunoassay Test Kits | On-site analytical tools for detecting specific contaminants (e.g., PCBs, pesticides). Used for rapid screening and verification of surface decontamination efficacy, providing results in under an hour [49]. |
| Sterile Wipe Sampling Kits | Pre-packaged kits containing sterile filters and templates for standardized surface sampling. Used to collect chemical or microbial contaminants from surfaces for quantitative analysis to verify cleaning effectiveness [49]. |
FAQs: Controlling Contamination in Surface Measurement Research
1. What is the Hierarchy of Controls and why is it the preferred strategy for contamination control?
The Hierarchy of Controls is a system used to prioritize actions for reducing or eliminating hazardous workplace exposures, with the most effective protections at the top. It is the preferred strategy because it provides a structured framework to select the most robust and reliable controls, rather than relying on methods that require constant human intervention. The preferred order, from most to least effective, is:
- Elimination: Physically remove the hazard.
- Substitution: Replace the hazard with a safer alternative.
- Engineering Controls: Isolate people from the hazard.
- Administrative Controls: Change the way people work.
- Personal Protective Equipment (PPE): Protect the worker with protective equipment [59] [60].
Using this hierarchy ensures exposures are reduced at the source, providing more dependable and long-term protection for both personnel and research integrity than relying on PPE or procedural rules alone [59].
2. Which engineering controls are most critical for preventing cross-contamination of surfaces in a lab?
Several engineering controls are fundamental to preventing cross-contamination. The most critical include:
- Biological Safety Cabinets (BSCs): Enclosed, ventilated workspaces with HEPA filters that protect both the user and the sample from biological contaminants. They are essential for working with pathogens and must be certified annually [61].
- Chemical Fume Hoods: Designed to capture and remove hazardous dusts, gases, vapors, and fumes generated within them, protecting the lab worker and environment. They are extremely effective when used properly [61].
- Laminar Flow Clean Benches: Provide a sterile, particulate-free workspace by passing HEPA-filtered air across the work surface in a laminar flow. Important note: These benches protect the product but do not protect the user, and should only be used for non-infectious, non-volatile materials [61].
- Local Exhaust Ventilation (e.g., "Snorkels"): Flexible exhaust arms that can be positioned close to a source of contamination to capture it before it disperses into the lab air [61].
- Dedicated Equipment and Workspaces: Using equipment for specific applications and establishing physically separated zones for different processes (e.g., clean vs. dirty, pre-PCR vs. post-PCR) prevents the transfer of contaminants between experiments [62].
3. Our team is processing low-biomass samples. What specific administrative controls should we implement?
Low-biomass samples are particularly susceptible to contamination, making stringent administrative controls essential [63]. Key procedures include:
- Rigorous SOPs: Develop and enforce detailed Standard Operating Procedures for sample collection, handling, processing, and decontamination. These should specify required PPE, engineering controls, and waste disposal procedures [64].
- Comprehensive Training: Train all personnel on the unique challenges of low-biomass research, including the sources of contamination (reagents, human skin, etc.) and the critical importance of adhering to every step of the SOPs [62] [63].
- Environmental Monitoring Program: Implement a routine schedule for surface sampling and testing using microbial (e.g., contact plates) and non-microbial (e.g., ATP bioluminescence) methods to verify the effectiveness of your cleaning regimens and monitor the lab environment [5].
- Strict Personal Hygiene Policies: Prohibit eating, drinking, applying cosmetics, and storing food in labs. Mandate frequent handwashing and the removal of lab coats and gloves before leaving the laboratory area [64].
- Meticulous Housekeeping: Maintain a clean and clutter-free laboratory. This includes immediate cleanup of spills, keeping storage organized, and ensuring exits and emergency equipment are unobstructed [64].
4. When is PPE an acceptable control method, and what does an effective PPE program include?
PPE is considered the last line of defense and is acceptable in the following situations:
- While other, more effective controls are being developed or implemented.
- When engineering and administrative controls cannot sufficiently reduce the hazardous exposure to safe levels.
- During emergency response or maintenance activities [59] [60].
An effective PPE program is more than just distributing equipment. It must include [59]:
- A thorough workplace hazard assessment to determine the necessary PPE.
- Proper selection of PPE based on the specific hazards.
- Training for employees on how to don, doff, use, and maintain their PPE.
- Regular inspection and replacement of damaged or worn-out equipment.
- Ongoing program monitoring to ensure its continued effectiveness.
Troubleshooting Guides
Problem: Inconsistent or skewed results in low-biomass sample analysis.
| Possible Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Contaminated reagents or labware | Run negative controls (e.g., sterile water through DNA extraction, unused swabs). Sequence these controls. | Use dedicated, DNA-free reagents and consumables. Decontaminate surfaces and equipment with 80% ethanol followed by a nucleic acid degrading solution (e.g., bleach) [63]. |
| Cross-contamination between samples | Review workflow for physical proximity of high- and low-biomass samples. Check for aerosol generation during pipetting. | Re-organize lab workflow spatially and temporally to separate clean and dirty processes. Use positive displacement pipettes and filtered tips. Implement rigorous cleaning between sample handlings [63]. |
| Inadequate engineering controls | Verify certifications for Biosafety Cabinets and fume hoods. Check for drafts that disrupt airflow. | Ensure annual certification of all hoods and cabinets. Keep hood sashes at proper operating height. Maintain equipment per manufacturer specifications [61]. |
| Personnel-derived contamination | Audit PPE and glove-changing practices. Use sampling controls (e.g., swabs of gloves, PPE) [63]. | Enforce consistent use of appropriate PPE (gloves, lab coats, masks). Train staff to change gloves frequently and avoid touching personal items or surfaces after donning gloves [62] [64]. |
Problem: Recurring chemical exposure incidents during surface application tasks.
| Possible Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Reliance on PPE over primary controls | Review current risk assessments and lab SOPs to determine if elimination, substitution, or engineering controls are feasible. | Substitute hazardous solvents with less toxic alternatives (e.g., water-based instead of solvent-based) [60]. Implement engineering controls like local exhaust ventilation ("snorkels") or use a fume hood for all procedures with volatile chemicals [61] [65]. |
| Ineffective or malfunctioning fume hood | Check hood airflow (e.g., with a tissue). Look for certification sticker. Note if alarms are active. | Report malfunctioning hoods to facilities immediately. Keep hood sashes closed when not in use. Ensure annual certification is current. Do not use a hood that is not functioning properly [61] [65]. |
| Poor administrative controls & work practices | Observe lab practices for clutter, improper chemical storage (open containers), and housekeeping. | Implement and enforce SOPs that specify safe work practices. Maintain good housekeeping. Keep all chemical containers sealed when not in use [64]. |
The Scientist's Toolkit: Key Reagents & Materials for Surface Contamination Control
| Item | Primary Function | Application Notes |
|---|---|---|
| ATP Bioluminescence Test Kits | Monitoring cleanliness by detecting residual organic matter (Adenosine Triphosphate) on surfaces [5]. | Provides rapid, real-time results. Effective for monitoring general surface soil, but not specific for microbial contamination [5]. |
| HEPA Filters | Removing particulates and microorganisms from air supplied to critical environments like BSCs and clean benches [61]. | Essential for creating ISO-classified clean zones. Integrity must be regularly tested and certified. |
| Nucleic Acid Degrading Solutions | Destroying contaminating DNA and RNA on surfaces and equipment to prevent false positives in molecular work [63]. | Sodium hypochlorite (bleach) is commonly used. Required for low-biomass microbiome studies to eliminate trace DNA [63]. |
| Microbial Surface Samplers | Directly analyzing surface microbial contamination (e.g., contact plates, swabs) [5]. | Used for specific microbial detection and enumeration. Can be used to track pathogen reservoirs or validate cleaning protocols [5]. |
| Sticky Mats | Capturing and retaining particulate contaminants from footwear at lab entry points [62]. | A simple but effective engineering control to minimize the transfer of dirt and microbes into sensitive areas. |
Experimental Protocol: Validating Surface Cleanliness Using an Integrated Approach
1.0 Objective To verify the effectiveness of a surface decontamination procedure by simultaneously detecting residual organic soil and microbial contamination.
2.0 Principle This protocol integrates two direct monitoring methods: ATP bioluminescence for immediate assessment of general cleanliness, and microbial contact plates for specific culturable microbiological assessment. This provides a more comprehensive validation than either method alone [5].
3.0 Materials
- ATP bioluminescence meter and compatible swabs.
- General-purpose microbial contact plates (e.g., Tryptic Soy Agar).
- Pre-defined sampling grid or template.
- Sterile gloves.
- Laboratory record sheet.
4.0 Procedure
- Pre-cleaning Baseline: Swab a defined area (e.g., 10x10 cm) of the surface to be validated using the ATP swab according to manufacturer instructions. Measure and record the Relative Light Units (RLU). Immediately after, press a contact plate onto the same defined area for the specified time (e.g., 10 seconds). Label the plate "Pre-cleaning."
- Perform Decontamination: Execute the standard surface decontamination procedure (e.g., disinfectant wipe-down).
- Post-cleaning Verification: After the prescribed contact time for the disinfectant, repeat step 1 on the same, now-cleaned surface area, using new ATP swabs and a new contact plate. Label these "Post-cleaning."
- Incubation: Incubate the contact plates as required (e.g., 30-35°C for 24-48 hours).
- Analysis: Count the colony-forming units (CFU) on the pre- and post-cleaning contact plates. Compare the pre- and post-cleaning RLU and CFU values against pre-established action limits for the specific facility [5].
Control Hierarchy for Contamination Prevention
The diagram below illustrates the logical relationship between the levels of the Hierarchy of Controls and their application in a research setting.
Leveraging Monitoring Data for Continuous Quality Improvement and Cleaning Validation
This technical support center provides troubleshooting guides and FAQs to help researchers, scientists, and drug development professionals address contamination problems in surface measurements research.
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between cleaning validation and cleaning verification? A1: Cleaning validation is a pre-approved, systematic study that provides documented evidence that a cleaning procedure consistently and effectively removes residues to a predetermined acceptable level, ensuring quality for future batches. In contrast, cleaning verification is a routine, batch-specific check conducted after cleaning to confirm that a particular piece of equipment is clean against set criteria for immediate use [66] [67].
Q2: Why can't we rely solely on visual inspection to confirm a surface is clean? A2: Visual inspection alone is ineffective because many contaminants are invisible to the naked eye at concentrations that can still pose a significant risk. Residues of active pharmaceutical ingredients (APIs), microorganisms, or cross-contaminants must be reduced to levels established by scientific rationale, which requires analytical testing [68] [67]. Furthermore, high-touch surfaces often exhibit moderate contamination levels that are not visually detectable but can still act as key nodes in microbial transmission [14].
Q3: How often should cleaning validation be repeated? A3: After the initial validation, a program should be in place to ensure each piece of equipment is reassessed at least once every three years [67]. Revalidation is also required when significant changes occur, such as a new product introduction, major equipment modification, or change in cleaning procedure [66].
Q4: What is a "worst-case" product, and why is it important in validation? A4: A worst-case product is one that presents the greatest challenge to the cleaning process, typically due to factors like poor solubility of the API, high potency/toxicity, or a formulation that is particularly difficult to remove from equipment surfaces. Validating with this product provides assurance that the cleaning procedure will be effective for all products in a similar group [67].
Troubleshooting Guides
Guide 1: Addressing Consistently Failed Cleaning Validation Tests
If your sampling results consistently fail to meet the predetermined acceptance criteria, follow this systematic approach.
Step 1: Investigate the Sampling and Analytical Methods
- Confirm that the sampling recovery study has been properly validated for the specific surfaces and residues being tested.
- Verify that the analytical methods are specific, sensitive, and calibrated for the analytes (e.g., specific API, cleaning agent).
- Check the sampling technique itself; improper swabbing or rinse procedures can lead to inaccurate results [67].
Step 2: Review the Cleaning Procedure Execution
- Audit the execution of the cleaning procedure against the approved SOP. Look for deviations in parameters such as water quality, cleaning agent concentration, water temperature, contact time, and flow rates (for CIP systems) [66].
- Ensure that operators are thoroughly trained and that the documentation for critical cleaning steps is complete [68].
Step 3: Evaluate the Cleaning Procedure Design
- The current procedure itself may be inadequate. Assess if the cleaning agent is appropriate for the soil (e.g., is a detergent needed for an insoluble residue?).
- For manual cleaning, the variability is higher; consider if the procedure is overly complex or reliant on difficult-to-control manual effort [68] [66].
- Examine equipment design for hard-to-clean areas (e.g., ball valves, long transfer lines, internal crevices) that may be missed by the current procedure [68].
Step 4: Check for Process Changes
- Investigate if any changes were made to the manufacturing process that could have altered the nature of the soil (e.g., a change in an excipient or raw material supplier) without a corresponding update to the cleaning procedure [67].
Guide 2: Handling Unexpected Contamination Findings on "Clean" Surfaces
This guide assists when routine monitoring or verification detects contamination on surfaces that have passed the cleaning process.
Step 1: Confirm the Result
- First, rule out false positives from laboratory error or sample contamination. Re-test any retained samples and check controls [67].
Step 2: Perform a Root Cause Analysis
- Source of Contamination: Identify the contaminant. Is it the previous product, a cleaning agent, a microbial biofilm, or an unknown impurity? This will guide the investigation.
- Vector of Spread: Determine how the contamination occurred. Consider these common vectors:
- Inadequate Cleaning: The cleaning procedure did not effectively remove the residue.
- Post-Cleaning Contamination: The equipment was contaminated after the cleaning process was complete. Investigate clean and dirty hold times, storage conditions, and handling practices [68].
- Cross-Contamination: Contamination was introduced from another source, such as a shared utensil, improper gowning, or airborne particles [5] [68].
- Biofilm Presence: Microorganisms have established a biofilm, which is highly resistant to cleaning and sanitization agents [5].
Step 3: Implement Corrective and Preventive Actions (CAPA)
- Based on the root cause, implement immediate corrections (e.g., re-cleaning the affected equipment) and long-term preventive actions.
- This may involve revising SOPs, enhancing personnel training, modifying equipment, or revalidating the cleaning process [67].
Experimental Protocols for Surface Measurement Research
Protocol 1: Validating a Swab Sampling Recovery Study
This protocol is critical for ensuring that your surface sampling method accurately quantifies the residue present.
Objective: To determine the efficiency with which a specific residue (e.g., an API) is recovered from a specified surface material (e.g., stainless steel 316L) using a defined swabbing technique and analytical method.
Materials:
- Surfaces: Coupons of the same material as the production equipment.
- Swabs: Specified type (e.g., polyester, cotton).
- Solvent: Specified solvent for wetting the swab and for extraction.
- Analytical Standard: High-purity reference standard of the analyte.
- Instrumentation: Validated analytical instrument (e.g., HPLC, TOC analyzer).
Methodology:
- Preparation: Clean the coupons thoroughly and verify they are free of the analyte.
- Application: Apply a known, precise volume of a standard solution of the analyte to a defined area (e.g., 25 cm²) on the coupon surface. Allow the solvent to evaporate completely.
- Sampling: Swab the inoculated area using the approved SOP technique. Typically, this involves wetting the swab with solvent, swabbing in a systematic pattern (e.g., horizontally, vertically, and diagonally), and swabbing the same area with a second dry swab to capture remaining residue.
- Extraction: Place both swabs in a vial containing a known volume of extraction solvent. Shake or sonicate to extract the analyte.
- Analysis: Analyze the extracted solution using the designated analytical method.
- Calculation: Calculate the percentage recovery using the formula:
(Amount of analyte recovered / Amount of analyte applied) × 100.
Acceptance Criteria: Recovery efficiency should be consistent and high. While it depends on the analyte and surface, a recovery of >70-80% is often targeted to ensure the method is suitable for monitoring [67].
Protocol 2: Establishing a Surface Monitoring Program for Microbial Contamination
This protocol outlines how to set up an environmental monitoring program to track bioburden and prevent biofilm formation.
Objective: To routinely monitor the microbial contamination levels on critical equipment surfaces and in the environment to ensure they are controlled and to detect adverse trends.
Materials:
- Sterile swabs or contact plates (e.g., RODAC plates)
- Neutralizing buffer (if disinfectants are present on the surface)
- Incubator
Methodology:
- Site Selection: Identify sampling sites based on a risk assessment. Focus on areas after cleaning and sanitization. High-touch surfaces, zones closest to product contact surfaces, and hard-to-clean areas are often considered critical [5] [14].
- Sampling Frequency: Define a schedule (e.g., weekly, monthly, per campaign) based on the risk and data history.
- Sampling Technique:
- For Swabs: Use a sterile swab moistened with buffer. Swab a defined area (e.g., 10 cm x 10 cm). Aseptically transfer the swab to a tube of culture media.
- For Contact Plates: Gently press the agar surface onto the flat sampling site. Ensure full contact without sliding.
- Incubation: Incubate samples at appropriate temperatures (e.g., 20-25°C for mesophilic bacteria, 30-35°C for total aerobic count) for a specified duration.
- Data Recording: Count the colony-forming units (CFUs) and record them per unit area.
The table below summarizes the quantitative data and acceptance limits for a robust cleaning validation program.
| Validation Aspect | Parameter | Typical Acceptance Limit / Criteria | Reference / Rationale |
|---|---|---|---|
| Chemical Residue | API Carryover | ≤10 ppm or ≤1/1000 of normal therapeutic dose | Based on health-based exposure limits and analytical capability [68]. |
| Sampling Recovery | Swab Recovery Efficiency | Typically >70-80% | Ensures the sampling method is accurately quantifying residue [67]. |
| Process Consistency | Consecutive Successful Runs | 3 consecutive runs | Demonstrates that the cleaning process is consistent and reproducible [67]. |
| Microbiological | Bioburden | Based on product risk; specific CFU limits per contact plate or swab | Ensures control of microbial and endotoxin contamination [68]. |
| Visual Inspection | Surface Cleanliness | No visible residues | A qualitative but crucial first-line check [68]. |
The Scientist's Toolkit: Essential Research Reagents & Materials
The table below details key materials and solutions used in cleaning validation and surface contamination studies.
| Item | Function / Explanation |
|---|---|
| Polyester Swabs | Synthetic swabs are preferred over cotton as they are less likely to introduce interferents and have consistent release properties for analyte recovery [67]. |
| HPLC/UPLC with UV/FLD Detector | High-Performance Liquid Chromatography is the gold standard for specific quantification of low levels of Active Pharmaceutical Ingredients (APIs) in swab and rinse samples [66]. |
| Total Organic Carbon (TOC) Analyzer | A non-specific, highly sensitive method for detecting carbon-based residues from APIs, excipients, and cleaning agents. Ideal for a wide range of molecules and for water-for-injection (WFI) rinse water testing [66]. |
| Adenosine Triphosphate (ATP) Bioluminometer | Provides a rapid, real-time measurement of organic soil (including microbial contamination) on surfaces. Excellent for monitoring and verification, though not typically used for final validation due to its non-specificity [5]. |
| Neutralizing Buffer | Used in microbial sampling to inactivate any residual disinfectants (e.g., quaternary ammonium compounds, peroxides) on the sampled surface, ensuring an accurate count of viable microorganisms [5]. |
| Validated Cleaning Agent | A detergent or solvent with a known composition that is proven to be effective at removing the soil and is itself easily removable from equipment surfaces. Its use must be documented in an SOP [66] [67]. |
Workflow and System Diagrams
Cleaning Validation Lifecycle
Data Quality Feedback Loop
Frequently Asked Questions (FAQs)
What are false positives and false negatives in the context of surface measurements?
In surface measurement research, a false positive occurs when the analysis incorrectly indicates the presence of a contaminant or specific surface property that is not actually there. Conversely, a false negative occurs when the analysis fails to detect a contaminant or property that is present [69]. Both can significantly skew research outcomes and lead to incorrect conclusions in drug development.
How does environmental interference affect surface measurement accuracy?
Environmental factors such as ambient lighting, temperature fluctuations, humidity, and vibrational noise can introduce significant artifacts into sensitive surface measurements [69]. For instance, variable lighting can alter the perceived properties of a surface in image-based analysis, while temperature changes can affect the performance of measurement electronics and the material properties of the samples themselves, leading to unreliable data.
What is the "Base Rate Fallacy" and why is it important for researchers?
The Base Rate Fallacy describes the tendency to ignore the underlying statistical prevalence (base rate) of a condition when interpreting the results of a test. In contamination research, if the actual probability of contamination is very low, even a highly accurate test can produce a high number of false positives relative to true positives. Researchers must account for this to correctly interpret their findings and avoid being misled by positive results [69].
What are common sources of operator error in experimental protocols?
Operator error often stems from deviations from Standard Operating Procedures (SOPs), such as skipping steps, performing actions out of sequence, or incorrect timing [70]. Other sources include fatigue, especially during long experiments or late shifts, and misinterpretation of complex or unclear work instructions. These errors are often situational and can be correlated with specific contexts like shift handovers or high workload periods [70].
Troubleshooting Guides
Guide 1: Mitigating False Positives and False Negatives
False results compromise data integrity. This guide outlines a systematic approach to identify and reduce their occurrence.
Problem: High rate of false positives in detection assays.
- Solution: Review and optimize your buffer system. Conventional ELISA and other assay buffers can cause intense non-specific reactions due to the hydrophobic binding of immunoglobulins to plastic surfaces. Transition to a buffer specifically formulated to reduce this "background (BG) noise reaction" without interfering with specific antigen-antibody interactions [71].
- Actionable Steps:
- Include antigen non-coated blank wells in your assay to determine the background noise level for each individual sample [71].
- Systematically compare the performance of your current buffer against a specialized blocking buffer like ChonBlock to quantify the reduction in non-specific binding.
- Validate any new buffer system with known positive and negative control samples to ensure specificity is maintained.
Problem: High rate of false negatives, missing existing contaminants.
- Solution: Implement a change-detection approach in your analysis. This involves comparing current measurement data with a baseline reading from a known "clean" or control state. This helps to highlight deviations that signify true positives [69] [72].
- Actionable Steps:
- Establish a robust and well-characterized baseline for your surface.
- Use analytical techniques, such as those employed in Synthetic Aperture Radar (SAR) flood mapping, which compare pre-event and during-event images to isolate the true signal from noise [72].
- Correlate results with auxiliary data sources (e.g., temperature logs, vibration sensor data) to confirm findings.
Problem: Results are skewed due to the low base rate of actual contamination (Base Rate Bias).
- Solution: Incorporate Bayesian statistical analysis into your data interpretation. This method explicitly accounts for the prior probability of contamination (the base rate) to calculate the true probability that a positive result is correct [69].
- Actionable Steps:
- Estimate the base rate of contamination in your specific research context from historical data.
- Use Bayes' theorem to update the probability of contamination given a positive test result, using your assay's known sensitivity and specificity.
Guide 2: Correcting for Environmental Interference
Environmental factors introduce noise that can obscure genuine measurement signals.
Problem: Measurements are inconsistent due to variable ambient conditions.
- Solution: Create a controlled measurement environment and use environmental shielding.
- Actionable Steps:
- Conduct experiments in a temperature-controlled laboratory with stable humidity levels.
- Use Faraday cages or vibration-damping optical tables to isolate sensitive equipment from electromagnetic and vibrational noise.
- For image-based measurements, use consistent, diffuse lighting sources and operate in darkroom conditions where possible to eliminate ambient light fluctuations [69].
Problem: Data is corrupted by intermittent environmental noise.
- Solution: Employ sensor fusion and data filtering techniques.
- Actionable Steps:
- Install environmental sensors (e.g., thermometers, hygrometers, seismometers) to log conditions during every measurement.
- Post-process your data using algorithms (e.g., digital filters) to subtract or correct for the recorded environmental artifacts.
- Use sensing modalities that are less susceptible to specific interferences; for example, radar-based sensing can penetrate cloud cover and is effective in both day and night conditions, unlike optical methods [72].
Guide 3: Reducing Operator-Induced Error
Human error is a systemic issue that can be mitigated through improved processes and training.
Problem: Deviations from SOPs lead to inconsistent results.
- Solution: Implement digital work instructions and leverage AI for deviation detection.
- Actionable Steps:
- Replace paper-based SOPs with interactive digital checklists that guide the operator through each step.
- Use AI-powered software to analyze operator logs and task timestamps, flagging steps that are frequently skipped, performed out of sequence, or where duration deviates significantly from the standard [70].
- Establish a structured on-the-job training (OJT) program where experienced researchers coach new hires on proper techniques [73].
Problem: Errors spike during specific contexts (e.g., shift changes, complex procedures).
- Solution: Adopt context-aware error analysis and optimize workflow design.
- Actionable Steps:
- Use AI clustering algorithms to analyze error logs and correlate them with contextual data like time of day, operator ID, and task complexity to identify high-risk scenarios [70].
- Redesign workflows to minimize task-switching and cognitive overload during critical phases.
- Introduce microlearning refreshers—short, focused training modules—on error-prone procedures just before they are performed [73].
Data Presentation
Table 1: Quantitative Impact of Common Pitfalls on Measurement Systems
| Pitfall Category | Typical Impact on Precision | Common Occurrence Rate | Mitigation Cost Level |
|---|---|---|---|
| False Positives | Can reduce precision by 15-30% in low base rate scenarios [69] | High in systems with low specificity buffers [71] | Medium (requires buffer optimization/validation) |
| False Negatives | Leads to >90% missed detections in worst-case scenarios [69] | Varies with sensor sensitivity and environmental noise [69] | High (may require sensor upgrades) |
| Environmental Interference | Can introduce 5-20% signal noise [69] | Very High in non-controlled labs | Low to High (shielding vs. environmental control) |
| Operator Deviation from SOP | Increases outcome variability by up to 50% across shifts [70] | Common in complex, high-fatigue contexts [70] | Medium (digital SOPs & training) |
Table 2: Essential Research Reagent Solutions for Contamination Control
| Reagent / Material | Primary Function | Application Note |
|---|---|---|
| Specialized Blocking Buffer (e.g., ChonBlock) | Reduces non-specific hydrophobic binding to plastic surfaces, minimizing false positives in plate-based assays [71]. | Essential for ELISA workflows using human serum; outperforms conventional buffers in reducing background noise [71]. |
| High-Purity Solvents & Diluents | Ensure no particulate or chemical contaminants are introduced during sample preparation or dilution. | Use HPLC-grade or higher solvents. Filter all buffers and solutions with 0.22 µm filters before use. |
| Validated Negative Control Samples | Provides a baseline measurement to distinguish true signal from system noise and background interference. | Must be subjected to the exact same protocol as test samples. Critical for calculating signal-to-noise ratios. |
| Synthetic Aperture Radar (SAR) Data | Enables consistent surface mapping and change detection unimpeded by cloud cover or lighting conditions [72]. | Used as a model for developing robust detection workflows resilient to environmental interference. |
Experimental Protocols
Protocol 1: Validating Assay Specificity to Minimize False Positives
This protocol is designed to systematically identify and quantify non-specific reactions in surface-binding assays.
- Plate Preparation: Coat two sets of wells with your target antigen. Leave a third set uncoated (blank wells).
- Buffer Comparison: Prepare sample dilutions using both a conventional buffer and a specialized blocking buffer (e.g., ChonBlock) [71].
- Sample Addition: Add the diluted samples to both the antigen-coated and blank wells. The blank wells are critical for measuring the "background (BG) noise reaction" caused by hydrophobic binding to the plastic [71].
- Incubation and Washing: Follow standard assay incubation and washing procedures.
- Signal Detection: Develop the assay and measure the signal in all wells.
- Data Analysis:
- The signal in the blank wells represents the false positive signal.
- The true specific signal is calculated as: Signal (Coated Well) - Signal (Blank Well).
- Compare the magnitude of the false positive signal and the signal-to-noise ratio between the two buffer systems.
Protocol 2: Change-Detection Workflow for Isolating True Signal
This methodology uses a baseline comparison to enhance the reliability of damage or contamination detection, inspired by SAR-based flood mapping techniques [72].
- Baseline Acquisition: Perform a high-fidelity surface measurement on a pristine or certified clean control sample. This establishes the reference state.
- Test Sample Acquisition: Perform the same measurement on the test sample under investigation, ensuring environmental conditions are as identical as possible to the baseline acquisition.
- Image/Data Registration: Align the test dataset perfectly with the baseline dataset.
- Change Detection Analysis: Subtract the baseline data from the test data. The resulting differential map highlights changes that have occurred, which are potential indicators of contamination or damage.
- False Positive Filtering: Apply auxiliary data or logical masks to the differential map. For example, exclude areas known to be prone to false signals (e.g., edges, inherent material variations) to refine the results [72].
Experimental Workflow and Signaling Pathways
Contamination Identification Workflow
Decision Pathway for Pitfall Mitigation
Evaluating and Validating Detection Technologies and Procedures
For researchers tackling contamination problems in surface measurements, understanding the capability of your analytical methods is paramount. This guide defines the key performance metrics—the Limit of Detection (LOD) and Limit of Quantitation (LOQ)—and provides clear, actionable protocols to determine them, ensuring your data is both reliable and defensible.
What are the fundamental definitions of LOD and LOQ?
The Limit of Detection (LOD) and Limit of Quantitation (LOQ) are critical figures of merit that define the sensitivity of an analytical method. They describe the lowest concentrations of an analyte that can be reliably detected and quantified, respectively [74] [75].
- Limit of Detection (LOD): The lowest concentration of an analyte that can be reliably distinguished from a blank sample or the background noise, but not necessarily quantified with a specific degree of accuracy [74] [76]. It is the point at which you can say, "Yes, the analyte is present."
- Limit of Quantitation (LOQ): The lowest concentration of an analyte that can be not only detected but also quantified with stated, acceptable levels of precision (imprecision) and accuracy (bias) [74] [77]. At or above the LOQ, you can confidently report a numerical value for the concentration.
A related term, the Limit of Blank (LoB), is often used in established protocols. The LoB is the highest apparent analyte concentration expected to be found when replicates of a blank sample containing no analyte are tested [74].
The relationship between these limits is consistent: the LoQ is always greater than or equal to the LOD, which is in turn greater than the LoB [74] [75]. The following workflow outlines the decision process for an analyte signal near these limits:
How are LOD and LOQ calculated using different standard methods?
There is no single universal protocol for determining LOD and LOQ, and different approaches can yield different results [78] [77]. The table below summarizes the most common calculation methods.
Table 1: Common Methods for Calculating LOD and LOQ
| Method | Basis of Calculation | Typical LOD Formula | Typical LOQ Formula | Key Considerations |
|---|---|---|---|---|
| Signal-to-Noise (S/N) [79] [75] [76] | Ratio of analyte signal to background noise. | S/N = 3 or 2 | S/N = 10 | Quick, instrumental estimate. Does not account for full method precision or accuracy. |
| Blank Standard Deviation (IUPAC/ACS) [80] [75] | Standard deviation (SD) of replicate blank measurements. | LOD = Meanblank + 3*SDblank | LOQ = Meanblank + 10*SDblank | Requires an analyte-free blank. Can underestimate LOD if blank variance is low [81]. |
| Calibration Curve [77] | Standard error of the regression (Sy/x) and slope (m). | LOD = 3.3 * Sy/x / m | LOQ = 10 * Sy/x / m | Common in chromatography. Uses data from the calibration process itself. |
| Clinical & Laboratory Standards Institute (CLSI) EP17 [74] | Uses both blank samples and low-concentration samples. | LOD = LoB + 1.645*SDlow concentration sample | LOQ ≥ LOD, defined by meeting precision/bias goals | Rigorous, empirical protocol. Provides a reliable estimate supported by experimental data [74] [81]. |
What are the best practices and troubleshooting tips for determining LOD/LOQ?
Troubleshooting Common Issues:
- My calculated LOD seems too optimistic (low).
- Cause: Using only the standard deviation of a pure solvent blank, which may not capture the variability of a real sample matrix [80].
- Solution: Use a method blank that incorporates all reagents and sample processing steps. Alternatively, adopt the CLSI EP17 approach that uses a low-concentration sample to capture true method imprecision [74] [81].
- I get different LOD/LOQ values when using different calculation methods.
- Cause: This is expected, as the methods are based on different statistical principles and assumptions [78] [77].
- Solution: Consistently report which method and confidence level (e.g., k=3 for 99% confidence) you used. For method validation, choose the approach mandated by your governing regulatory body or standard.
- I cannot obtain a true analyte-free blank for my complex sample matrix.
- Cause: This is a common challenge when analyzing endogenous analytes or complex environmental samples [77].
- Solution: Use the method of standard additions (fortification) to prepare samples with low levels of analyte. The LOD/LOQ can then be determined from the calibration curve built from these fortified samples [77] [81].
- How can I achieve the lowest possible LOD for my surface contamination analysis?
- Minimize Contamination: Use high-purity reagents, perform sample preparation in a laminar flow box, and use conditioned containers to prevent leaching [79].
- Optimize Instrumentation: Tune your instrument (e.g., ICP-MS, XPS) for maximum sensitivity and minimal background. This can include optimizing plasma conditions, ion optics, and using collision-reaction cells to remove interferences [79] [82].
- Advanced Strategies: For techniques like LIBS, advanced optimization algorithms (e.g., Bayesian optimization) can systematically find instrument parameters that yield the highest sensitivity and lowest LOD [83].
Detailed Experimental Protocols
Protocol 1: Determining LOD and LOQ via the CLSI EP17 Empirical Method [74]
This protocol is considered robust because it tests the method's performance with actual analyte present.
- Sample Preparation:
- Prepare a minimum of 60 replicates of a blank sample (contains no analyte).
- Prepare a minimum of 60 replicates of a low-concentration sample (e.g., a dilution of your lowest calibrator, expected to be near the LOD).
- Note: For laboratory verification (as opposed to initial establishment), 20 replicates of each may be sufficient.
- Analysis:
- Analyze all blank and low-concentration sample replicates in a randomized sequence, treating them identically to real patient or test samples.
- Data Analysis and Calculation:
- Calculate LoB: LoB = Meanblank + 1.645 * SDblank
- Calculate LOD: LOD = LoB + 1.645 * SDlow concentration sample
- Verify LOD: Ensure that no more than 5% of the results from the low-concentration sample fall below the LoB. If more than 5% fail, the LOD is too low and must be re-estimated using a sample with a higher concentration.
- Determine LOQ: Test samples at or just above the LOD concentration. The LOQ is the lowest concentration at which your method meets pre-defined goals for bias and imprecision (e.g., total error ≤ 20%).
Protocol 2: Determining LOD and LOQ from a Calibration Curve [78] [77]
This method is efficient as it uses data typically generated during method validation.
- Calibration:
- Prepare a calibration curve with a minimum of 5 concentrations across your expected range. The lowest standard should be near the expected LOQ.
- Analyze each calibration level in replicate (e.g., 3-5 times).
- Regression Analysis:
- Perform a linear regression on the data (y = signal, x = concentration) to obtain the slope (m) and the standard error of the regression (Sy/x).
- Calculation:
- LOD = (3.3 * Sy/x) / m
- LOQ = (10 * Sy/x) / m
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Low-Level Contamination Analysis
| Item | Function | Considerations for Low LOD Work |
|---|---|---|
| High-Purity Acids & Reagents | Sample digestion, dilution, and stabilization. | Source ultrapure grades (e.g., TraceMetal Grade) to minimize background contamination from the reagents themselves [79]. |
| Laminar Flow Box / Clean Bench | Provides a controlled environment for sample prep. | Drastically reduces airborne particle contamination from the laboratory environment during critical preparation steps [79]. |
| PFA or PTFE Labware | Sample containers, vials, and beakers. | These materials are resistant to leaching and adsorption. Condition all labware with a dilute acid (e.g., 1% HNO3) before first use [79]. |
| HEPA-Filtered Autosampler Covers | Encloses the autosampler. | Minimizes the introduction of dust and contaminants while samples are waiting to be analyzed in the instrument [79]. |
| Certified Reference Materials | Method validation and quality control. | Use matrix-matched reference materials with certified values at low concentrations to verify your method's accuracy and LOD/LOQ claims. |
How do I account for uncertainty near the detection limit?
Measurements near the LOD and LOQ are associated with high statistical uncertainty [82]. It is crucial to understand and report this uncertainty.
- For Quantitative Reports: Do not report precise numerical values for samples with concentrations below the LOQ. Instead, use descriptive terms such as "< LOQ" or "not detected (LOD = [value])" [76].
- Uncertainty Estimation: For results near the LOQ, the measurement uncertainty can be estimated and reported as a range (e.g., 10 ± 3 μg/L). Advanced statistical approaches, like the uncertainty profile, which is based on tolerance intervals, can provide a more realistic assessment of uncertainty across the measurement range, especially at low concentrations [78].
- Background Subtraction: In techniques like XPS, the method used to subtract the spectral background significantly impacts the peak area uncertainty near the detection limit. Using correlated background points can lead to a more accurate estimation of this uncertainty [82].
The accurate detection and measurement of surface contaminants are critical for public health, environmental safety, and drug development. Researchers face a complex landscape of analytical technologies, each with distinct strengths and limitations. This technical support center provides a structured comparison, detailed protocols, and troubleshooting guidance for three cornerstone methodologies: Immunoassays, Mass Spectrometry, and Direct-Reading Instruments. The content is framed within a broader thesis on resolving contamination problems in surface measurements, helping you select and optimize the right technology for your specific research challenges.
Technology Comparison at a Glance
The table below summarizes the core characteristics of each technology to guide your initial selection.
| Feature | Immunoassays | Mass Spectrometry (MS) | Direct-Reading Instruments |
|---|---|---|---|
| Key Principle | Antigen-antibody binding for molecular recognition [84] | Measurement of mass-to-charge ratio (m/z) of ionized analytes [85] | Often optical (e.g., fluorescence, Raman) for real-time analysis [86] |
| Typical Workflow | Multi-step, often involves washing and incubation [84] | Multi-step: sample prep, separation (LC/GC), ionization, detection [85] [87] | Minimal sample prep; direct, rapid measurement [86] |
| Sensitivity | High (e.g., FIA median LOD: ~1.5×10⁻¹¹ M) [84] | Very High (e.g., SERS IA median LOD: ~4.3×10⁻¹³ M) [84] | Varies; generally lower, suited for screening [86] |
| Specificity | High, but cross-reactivity can occur [87] | Excellent, based on molecular mass and fragmentation [85] | Can be lower; susceptible to matrix interference [86] |
| Throughput | High (e.g., ELISA, lateral flow) [84] | Moderate to High (especially with modern automation) [88] | Very High (real-time or near-real-time data) [86] |
| Quantitation | Semi-Quantitative to Fully Quantitative | Fully Quantitative (gold standard) [89] [85] | Semi-Quantitative to Quantitative |
| Best for | High-throughput screening, field use, cost-effective targeted analysis [90] | Definitive identification, ultra-trace level quantification, multi-analyte panels [90] [85] | Rapid screening, field measurements, process monitoring [86] |
Troubleshooting Guides & FAQs
Immunoassays
Q1: My immunoassay shows high background noise. What could be the cause? A1: High background is often caused by non-specific binding. To mitigate this:
- Increase Stringency: Optimize the concentration of blocking agents (e.g., BSA, non-fat dry milk) in your buffer.
- Improve Washing: Ensure washing buffers contain appropriate detergents (e.g., Tween-20) and that washing steps are thorough.
- Check Antibody Specificity: Verify the specificity of your primary and secondary antibodies. Titrate to find the optimal concentration that minimizes non-specific binding [84].
Q2: I am getting false-positive results. How can I address this? A2: False positives can arise from cross-reactivity with structurally similar compounds or matrix interference.
- Validate with MS: Use a mass spectrometry method to confirm positive results from immunoassays, as MS is less prone to such interference [87].
- Analyze Matrix: Test your assay with a blank matrix (without the analyte) to check for inherent interference. Sample purification or dilution may be necessary [90].
Mass Spectrometry
Q3: My LC-MS/MS signal is suppressed or enhanced. How do I fix these matrix effects? A3: Matrix effects are a common challenge in LC-MS/MS, caused by co-eluting compounds that alter ionization efficiency.
- Improve Chromatography: Optimize the LC method to achieve better separation of the analyte from potential interferents.
- Sample Cleanup: Incorporate a more rigorous sample preparation step, such as Solid Phase Extraction (SPE) or Micro-SPE [88].
- Use Isotopic IS: Employ a stable, isotopically labeled internal standard (IS). The IS experiences the same matrix effects as the analyte, allowing for accurate correction [85].
Q4: How can I ensure the quality and accuracy of my quantitative MS data? A4: Rigorous quality assurance (QA) is critical for clinical and regulatory applications.
- Internal QC: Analyze quality control (QC) samples at multiple concentrations daily. Use acceptance criteria based on the intended use of the test [85].
- Proficiency Testing: Participate in external QA or proficiency testing schemes where identical samples are analyzed by multiple laboratories [85].
- Method Validation: Thoroughly validate methods for parameters like linearity, precision, accuracy, and recovery before use [89].
General Workflow & Technology Selection
Q5: What is a typical end-to-end workflow for analyzing contaminants in a complex sample? A5: The following workflow diagram outlines a general pathway from sample collection to data analysis, highlighting steps that are common across technologies and those that are specific.
Q6: How do I choose between an immunoassay and mass spectrometry for my project? A6: The choice depends on your project's specific requirements for throughput, cost, and data certainty.
- Choose Immunoassay if: You need high-throughput, low-cost screening for a specific analyte, have access to a reliable kit, and do not require definitive confirmation. It is excellent for initial screening phases [84] [90].
- Choose Mass Spectrometry if: You require definitive identification and precise quantification, are analyzing multiple analytes simultaneously, or need to detect compounds at ultra-trace levels. It is the preferred method for confirmatory analysis and complex matrices [90] [85].
- Hybrid Approach: A powerful strategy is to use immunoassays for rapid screening and then confirm positive or borderline samples using mass spectrometry [89].
Essential Research Reagent Solutions
The table below lists key reagents and materials crucial for successful experiments in this field.
| Reagent/Material | Function | Example Use Cases |
|---|---|---|
| Certified Reference Materials (CRMs) | Method validation and calibration to ensure analytical trueness [91]. | Quantifying mycotoxins in food/ herbal samples; calibrating heavy metal analysis [91]. |
| Stable Isotope-Labeled Internal Standards | Corrects for sample loss and matrix effects in quantitative MS [85]. | LC-MS/MS quantitation of drugs, metabolites, and contaminants in biological fluids [85]. |
| Monoclonal/Polyclonal Antibodies | Provides high specificity for target analyte recognition in immunoassays [84]. | Developing ELISA kits for pesticide detection or lateral flow tests for pathogens [84] [87]. |
| Surface-Enhanced Raman Scattering (SERS) Substrates | Amplifies Raman signal for highly sensitive detection, often in direct-reading tools [86] [84]. | Building biosensors for environmental pollutants or disease biomarkers [86] [84]. |
| Solid Phase Extraction (SPE) Sorbents | Purifies and pre-concentrates analytes from complex matrices, reducing interference [88]. | Cleaning up environmental water samples prior to PFAS analysis by LC-MS/MS [88]. |
Detailed Experimental Protocols
Protocol 1: Automated PFAS Analysis in Environmental Samples via LC-MS/MS
This protocol leverages automation to address the significant challenges in analyzing Per- and Polyfluoroalkyl Substances (PFAS), as highlighted in recent presentations [88].
1. Sample Preparation (Automated)
- Weigh & Extract: Accurately weigh the environmental sample (e.g., soil, water). Using an automated platform (e.g., PAL System), perform a solid-liquid extraction with a methanol/water mixture.
- Automated Cleanup: Integrate a Micro-Solid Phase Extraction (Micro-SPE) step on the same automated platform to purify the extract and concentrate the PFAS analytes, removing interfering matrix components [88].
2. LC-MS/MS Analysis
- Chromatography: Inject the purified extract into a reversed-phase LC system. Use a mobile phase gradient of ammonium acetate in water and methanol to achieve optimal separation of various PFAS compounds.
- Mass Spectrometry: Operate the mass spectrometer in negative electrospray ionization (ESI-) mode. Use Multiple Reaction Monitoring (MRM) for sensitive and selective detection. Monitor specific precursor → product ion transitions for each target PFAS [88].
3. Data Quantification
- Calibration: Use a calibration curve prepared with PFAS certified reference standards in a blank matrix.
- Compliance: Quantify concentrations against the curve and compare to regulatory limits as defined in methods like EPA 1633 [88].
Protocol 2: Validating an Immunoassay with Mass Spectrometry
This protocol is crucial when using an immunoassay for a critical application, such as clinical diagnosis or regulatory safety testing [89].
1. Parallel Sample Analysis
- Split Samples: Divide a set of patient or sample extracts (e.g., urine for cortisol analysis) into two aliquots [89].
- Run Immunoassay: Analyze one aliquot using the standard commercial or in-house immunoassay protocol (e.g., on a Roche, Mindray, or Snibe platform).
- Run LC-MS/MS: Analyze the second aliquot using a validated LC-MS/MS method. This method serves as the reference standard due to its superior specificity [89].
2. Statistical Comparison & Bias Assessment
- Correlation Analysis: Calculate the Spearman correlation coefficient to assess the relationship between the two methods [89].
- Regression & Bias: Perform Passing-Bablok regression and Bland-Altman plot analyses. This will identify any constant or proportional bias (systematic over- or under-estimation) present in the immunoassay results compared to the LC-MS/MS results [89].
3. Cut-off Determination & Implementation
- ROC Analysis: Use Receiver Operating Characteristic (ROC) curve analysis to determine the optimal diagnostic cut-off value for the immunoassay, using the LC-MS/MS results as the truth standard [89].
- Adopt New Cut-off: Implement the newly defined, method-specific cut-off value in all future clinical or research applications of that particular immunoassay kit to ensure accurate decision-making [89].
Troubleshooting Common Monitor Issues
Q: My surface contamination monitor is showing inconsistent readings between different measurements. What could be the cause?
A: Inconsistent readings can stem from several sources. First, verify that your calibration is current and traceable to national standards, as discrepancies between laboratories are known to occur even with proper traceability [92]. Check for localized contamination on your calibration reference sources or diffuse panels; even small contaminated areas can introduce significant systematic errors into your measurements [93]. Ensure environmental conditions are stable, as factors like temperature fluctuations and humidity can affect detector response. Finally, perform a visual inspection of detectors and cables for any physical damage.
Q: After an annual calibration, our monitor fails its daily source check. What steps should we take?
A: This situation suggests a potential issue with the calibration procedure or instrument stability. First, contact your calibration service provider to verify the calibration was performed correctly and discuss the specific failure mode. Check whether the instrument underwent any repairs or maintenance just before calibration, as it should always be recalibrated after service work [94]. Review the calibration certificate to ensure the correct radionuclide standards were used for your specific application, as different nuclides (e.g., Sr-90, Cl-36, Cs-137, Co-60, Am-241) have different emission characteristics [92]. If the problem persists, the instrument may require more frequent calibration due to heavy usage or operating in challenging environmental conditions [94].
Q: What is the recommended frequency for calibrating surface contamination monitors?
A: For most regulatory compliance situations, portable radiation survey instruments must be calibrated at intervals not to exceed 12 months [94]. However, instruments used frequently in harsh environments (high humidity, extreme temperatures, dusty conditions) or subject to rough handling may require more frequent calibration—some facilities implement six-month or even quarterly schedules [94]. Always recalibrate after any repair or suspected malfunction [94]. Consult your manufacturer's recommendations as some may suggest specific intervals based on model and intended use.
Q: How can I verify the traceability of my calibration standards?
A: Proper traceability requires that reference sources be calibrated against national standards with documented continuity. Request calibration certificates from your provider that explicitly state traceability to national metrology institutes (like NIST) through an unbroken chain of comparisons [95]. For participation in international comparisons, look for evidence that your calibration laboratory is a member of organizations like EURAMET (The European Association of National Metrology Institutes), which ensures measurement comparability across borders [92].
Calibration Methodology and Reference Standards
Experimental Protocol: Efficiency Calibration in 2π Steradian Geometry
This protocol is based on comparative methods used by national metrology institutes for calibrating surface contamination monitors [92].
Purpose: To determine the detection efficiency of α, β surface contamination monitors in 2π geometry using traceable reference sources.
Materials and Equipment:
- Surface contamination monitor to be calibrated
- Traceable reference sources (e.g., Sr-90, Cl-36, Cs-137, Co-60 for β; Am-241 for α)
- Reference detector system (if performing comparative measurements)
- Distance fixtures for precise source-to-detector positioning
- Environmental monitoring equipment (temperature, pressure, humidity)
- Low-background shielding materials
Procedure:
- Pre-calibration Setup: Allow all equipment to stabilize in the measurement environment for at least 24 hours. Record environmental conditions.
- Background Measurement: Perform background measurements without sources present. For low-level measurements, use appropriate shielding.
- Source Measurement: Position each reference source at the prescribed calibration distance from the detector surface. Ensure consistent geometry for all measurements.
- Data Acquisition: For each source, collect counts for a sufficient duration to achieve statistical uncertainty < 2% (typically 10,000-100,000 counts).
- Efficiency Calculation: Calculate efficiency (ε) using the formula: ε = (Rnet / A) × 100%, where Rnet is the net count rate (gross minus background) and A is the surface emission rate of the source.
- Uncertainty Evaluation: Calculate measurement uncertainty considering components from counting statistics, source positioning, background subtraction, and reference source activity uncertainty.
- Validation: Verify calibration using a check source with known activity but different from calibration sources.
Table: Reference Radionuclides for Calibration [92]
| Radionuclide | Radiation Type | Typical Energy | Application Notes |
|---|---|---|---|
| Am-241 | α | 5.5 MeV | Alpha contamination monitoring |
| Sr-90 | β | 2.3 MeV (max) | High-energy beta calibration |
| Cl-36 | β | 0.7 MeV (max) | Medium-energy beta calibration |
| Cs-137 | β, γ | 0.5 MeV (max) | Gamma and beta monitoring |
| Co-60 | β, γ | 0.3 MeV (max) | Gamma and beta monitoring |
The Researcher's Toolkit: Essential Calibration Materials
Table: Key Research Reagent Solutions for Surface Contamination Studies
| Item | Function | Application Context |
|---|---|---|
| Traceable Reference Sources (α, β) | Provide known emission rates for efficiency calibration | Essential for establishing measurement traceability to national standards [95] |
| Standard Diffuse Panels | Serve as reflectance reference for optical systems | Critical for hyperspectral imaging calibration; requires regular cleaning and replacement [93] |
| Certified Buffer Solutions | pH calibration and verification | Used in hazardous drug contamination monitoring systems [55] |
| Contamination Check Sources (e.g., Sr-90, Am-241) | Daily functionality verification of monitors | Required for periodic performance checks between calibrations [92] |
| NIST-Traceable Calibration Weights | Mass measurement verification | Critical for analytical balance calibration in pharmaceutical applications [96] |
| Lateral Flow Immunoassay Cartridges | Rapid detection of specific hazardous drugs | Used in systems like BD HD Check for surface contamination monitoring [55] |
Calibration Workflow and Decision Pathways
Calibration Decision Workflow
Advanced Troubleshooting FAQs
Q: Our automated hyperspectral imaging system shows decreasing radiometric calibration accuracy between maintenance cycles. What solutions exist beyond manual cleaning?
A: For automated systems where manual cleaning is impractical, consider implementing a contamination-aware empirical line method (CA-ELM). This approach combines spectral feature clustering with spatial edge detection to automatically identify and exclude contaminated areas of standard diffuse panels, using only clean regions for calibration [93]. Studies show CA-ELM can reduce average reflectance error from 4.58% to 3.08% in locally contaminated panels, approaching performance achievable with clean panels [93]. Additionally, explore protective covers or automated cleaning mechanisms for diffuse panels to extend maintenance intervals.
Q: How significant are calibration discrepancies between different accredited laboratories?
A: Recent comparison exercises reveal that efficiencies in 2π steradian measured by different laboratories do not always agree despite proper traceability to primary standards [92]. These discrepancies are likely due to variations in calibration procedures rather than differences in primary standard measurements, suggesting that measurement uncertainties may be underestimated in some cases [92]. This highlights the importance of participating in comparison exercises and thoroughly reviewing calibration methodologies when selecting service providers.
Q: What quality control measures should we implement between formal calibrations?
A: Implement a comprehensive between-calibration QC program including:
- Daily source checks using traceable check sources to verify instrument functionality
- Routine background measurements to monitor for environmental changes
- Periodic intercomparisons between identical monitors
- Proficiency testing with known samples when available
- Strict documentation of all QC activities and investigation of any trends
Regular accuracy checks don't replace formal calibration but help detect early signs of instrument drift or malfunction [94].
FAQs: Multicentric Studies and Contamination Thresholds
Q1: What is the primary challenge in comparing contamination rates across different research centers? The primary challenge is the lack of a standardized definition for what constitutes contamination. A recent multicenter study of 52 U.S. hospitals found that institutions use different criteria from organizations like the College of American Pathologists (CAP), the Clinical and Laboratory Standards Institute (CLSI), or locally defined criteria. This variation means that the same data can yield different contamination rates, making accurate benchmarking between centers unreliable [97] [98].
Q2: How does the definition of contamination impact reported rates? The choice of definition directly impacts the calculated contamination rate. For example, when the study applied the CAP criteria, the mean blood culture contamination (BCC) rate in critical care units was 1.38%. However, when the same data was analyzed using the expanded National Healthcare Safety Network (NHSN) list of skin commensals, the rate was higher at 1.49%. This demonstrates that some facilities may appear to be within target levels while their true contamination rates are above recommended thresholds [97].
Q3: What are the proven consequences of high contamination rates in clinical studies? High contamination rates have significant downstream effects on data integrity and patient outcomes. The multicenter study found that for every 1% increase in the blood culture contamination rate, there was a associated 9% increase in central-line associated bloodstream infections (CLABSIs). Contaminated samples also lead to unnecessary antibiotic use, delayed or missed diagnoses, longer hospital stays, and substantially increased healthcare costs, estimated at $2,923–$5,812 per false positive [97] [98].
Q4: What strategies were identified to effectively reduce contamination rates? The study identified several key strategies associated with lower contamination rates:
- Monitoring blood culture volume (Adjusted OR: 0.26).
- Sharing blood culture data with clinical units (Adjusted OR: 0.19).
- Using electronic decision support tools to limit blood culture draws from central catheters (Adjusted OR: 0.12) [98].
Q5: Beyond microbial contamination, what other types of contamination threaten experimental data? In analytical chemistry and cell culture, other significant contamination types include:
- Chemical Contamination: From impurities in water, acids, and labware, which can introduce trace elements like lead or chromium [2].
- Cellular Contamination: Such as mycoplasma, which infects an estimated 5-30% of cell cultures without causing media turbidity, potentially altering cell metabolism and causing chromosomal aberrations [99].
- Viral Contamination: One study found a viral contamination incidence of over 25% in common cell lines, which often evades detection without specific testing [99].
Troubleshooting Guides
Guide 1: Troubleshooting High Contamination Rates in Multicentric Studies
| Problem | Possible Cause | Recommended Action | Validation Method |
|---|---|---|---|
| Inconsistent contamination rates across participating centers. | Use of different definitions and criteria for a contamination event. | Adopt a single, universal surveillance definition (e.g., the expanded NHSN commensal list) for all sites. | Recalculate all site rates using the new standardized definition and compare. |
| Inability to benchmark performance against other institutions. | Lack of a universal target threshold for contamination rates. | Establish a consensus threshold (e.g., ≤1%) for the entire research network or consortium. | Use statistical process control charts to monitor performance against the new benchmark. |
| Persistently high rates despite protocol updates. | Inconsistent feedback of contamination data to the personnel performing the procedures. | Implement a structured process for reporting contamination rates by unit and patient population. | Track the correlation between data feedback and contamination rate trends. |
| High rates of single blood cultures. | Phlebotomy practices that do not follow the recommended 4-bottle collection for adults. | Provide education and implement electronic decision support to optimize collection protocols. | Monitor the percentage of single blood cultures; target <5% [98]. |
Guide 2: Troubleshooting General Laboratory Contamination
| Problem | Possible Cause | Recommended Action | Validation Method |
|---|---|---|---|
| Unexpected trace elements in ICP-MS analysis. | Contaminated labware, water, or acids. | Use high-purity (e.g., ICP-MS grade) acids and FEP or quartz containers. Segregate labware for high/low concentration use [2]. | Analyze procedural blanks to identify the contamination source. |
| Cell culture decline without visible turbidity. | Mycoplasma contamination. | Implement routine screening using PCR, DNA staining, or mycoplasma culture methods. Avoid routine use of antibiotics [99]. | Perform a direct DNA stain (e.g., DAPI) and view with fluorescence microscopy. |
| Chemical contamination from surfaces. | Inadequate cleaning and disinfection of the lab environment. | Use ATP bioluminescence or protein swab tests to monitor surface cleanliness, not just visual assessment [5]. | Establish acceptable ATP RLU thresholds and track trends. |
Experimental Protocols for Contamination Monitoring
Protocol 1: Standardized Surface Sampling for Microbial Contamination
Principle: This protocol outlines a method for monitoring microbial contamination on laboratory and processing surfaces to validate cleaning regimens and prevent cross-contamination.
Materials:
- Sterile swabs (e.g., cotton or synthetic)
- Neutralizing buffer (e.g., Dey-Engley broth)
- Standard plate count agar or selective media
- Incubator
Methodology:
- Sampling Strategy: Identify critical control points (e.g., bench tops, equipment handles, biosafety cabinets) using a risk-based approach.
- Sampling Technique: Moisten the swab in neutralizing buffer. Swab a defined area (e.g., 10x10 cm) using a consistent pattern, rolling the swab between fingers. For irregular surfaces, ensure maximum contact.
- Elution: Aseptically place the swab in a tube containing a known volume of neutralizing buffer and vortex thoroughly to elute microorganisms.
- Plating and Incubation: Spread plate appropriate dilutions onto agar plates. Incubate under suitable conditions (e.g., 35°C for 48 hours) for bacterial counts.
- Calculation: Express results as Colony Forming Units (CFU) per unit area (e.g., CFU/cm²) [5].
Protocol 2: ATP Bioluminescence for Rapid Hygiene Monitoring
Principle: Adenosine Triphosphate (ATP) is present in all organic material. This assay uses luciferase to produce light in the presence of ATP, providing a rapid measure of surface soil.
Materials:
- ATP swab device and luminometer
- Clock or timer
Methodology:
- Sampling: Peel open the swab pouch and remove the device. Firmly swab a defined area using a consistent technique.
- Activation: Re-insert the swab into the device and break the valve to release the luciferase reagent.
- Measurement: Shake the device and insert it into the luminometer within 15 seconds. Record the result in Relative Light Units (RLUs).
- Interpretation: Establish action limits based on baseline readings from known-clean surfaces. High RLUs indicate inadequate cleaning [5].
Visualizing the Contamination Monitoring Workflow
Workflow for Contamination Control
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function | Considerations |
|---|---|---|
| High-Purity Water (ASTM Type I) | Diluent for standards and samples; cleaning final rinse. | Essential for trace-level analysis (ICP-MS). Must have low total organic carbon and resistivity of >18 MΩ-cm [2]. |
| ICP-MS Grade Acids | Sample digestion and preservation. | Certificates of Analysis should list elemental contamination levels. Nitric acid is generally cleaner than hydrochloric acid [2]. |
| Neutralizing Buffer | Used in swab sampling to neutralize residual disinfectants. | Prevents false negatives by allowing captured microorganisms to survive until plating [5]. |
| ATP Bioluminescence Assay | Rapid, non-microbial assessment of surface cleanliness. | Measures residual organic soil. Correlates with microbial load but is not a direct measure of viability [5]. |
| Mycoplasma Detection Kit | Routine screening for mycoplasma in cell cultures. | Methods include PCR, DNA staining (DAPI/Hoechst), and microbial culture. PCR offers speed and sensitivity [99]. |
| Fluorinated Ethylene Propylene (FEP) Labware | Storage and processing of samples for trace metal analysis. | Inert plastic that minimizes leaching of contaminants like boron, sodium, and silicon, which are common in glassware [2]. |
In surface measurements research, particularly in sensitive fields like pharmaceutical development, the integrity of data is paramount. Contamination, even at trace levels, can compromise years of research, lead to regulatory non-compliance, and result in significant financial losses. This technical support center provides a structured framework for researchers and scientists to evaluate the financial and operational merits of investing in advanced contamination control protocols. By quantifying both the immediate costs and the long-term benefits, organizations can make informed, defensible decisions that protect their research investments and ensure the reliability of their scientific findings.
The Cost-Benefit Analysis Framework
A Cost-Benefit Analysis (CBA) is a systematic, data-driven approach to evaluating a project's financial feasibility by comparing all anticipated costs against all expected benefits [100]. For contamination control, this means moving beyond the initial price tag of new equipment or processes and calculating the total cost of ownership against the value of risk reduction.
A Methodical Process
A robust CBA involves several key phases [101] [100]:
- Define the Project Scope: Clearly articulate the contamination control initiative. For example, instead of "improve lab cleanliness," specify "implement an automated pipette washing system to reduce elemental contamination in ICP-MS analysis for trace metal studies."
- Identify Costs and Benefits: Brainstorm with your project team to list all related costs and benefits, categorizing them as direct/indirect and tangible/intangible.
- Assign Monetary Values: Quantify each line item. While tangible items are straightforward, intangible benefits like reputational protection require estimation techniques.
- Calculate Net Present Value (NPV): Use the formula below to account for the time value of money. A positive NPV indicates a profitable project.
- Analyze Results and Decide: A positive NPV suggests the project is financially viable and should be accepted, while a negative NPV indicates it should be rejected [100].
The formula for calculating NPV is [100]: NPV = Σ [ (Bt - Ct) / (1 + i)^t ] Where:
B_t= Cash inflow (benefits) at time tC_t= Cash outflow (costs) at time ti= Discount rate (interest rate)t= Number of time periods
Quantifying Costs and Benefits
Investing in contamination control involves a mix of upfront and ongoing expenditures. The benefits, while sometimes intangible, are measurable with careful analysis.
Table 1: Comprehensive Cost-Benefit Breakdown for Contamination Control
| Category | Item | Description & Considerations |
|---|---|---|
| Costs | Non-Recurring Costs [101] | Initial capital investments and one-time purchases. |
| - Initial capital investment | Cost of new equipment (e.g., pipette washer, clean hood). | |
| - Equipment purchase | Analytical instruments, dedicated labware (FEP, quartz). | |
| - Security and privacy equipment | Access controls for clean rooms. | |
| - Software and licenses | For data management and analysis. | |
| - Space/Facilities | Modifications for a clean-room environment. | |
| - Research | Time spent validating new protocols. | |
| - Training | Initial sessions for personnel on new procedures. | |
| Recurring Costs [101] | Ongoing operational expenses. | |
| - Salaries | For personnel managing the systems. | |
| - High-purity acids & reagents | e.g., ICP-MS-grade nitric acid. | |
| - Supplies & Utilities | Consumables, high-purity water, energy for HEPA filters. | |
| - Equipment maintenance | Service contracts for specialized equipment. | |
| - Travel & Training | Refresher courses and conference attendance. | |
| - Overhead & Administrative | Allocated facility costs. | |
| Benefits | Tangible Benefits [101] | Measurable, direct financial gains. |
| - Reduced reagent costs | Less re-testing due to contaminated samples. | |
| - Fewer personnel hours | Less time spent troubleshooting contamination issues. | |
| - Reduced instrument downtime | Less maintenance required due to sample impurities. | |
| - Lower travel costs | Fewer on-site audits from regulators due to compliance. | |
| - Reduced regulatory fines | Avoidance of penalties for non-compliant data. | |
| Intangible Benefits [101] [2] | Critical advantages that are difficult to monetize but essential. | |
| - Reduced regulatory risk | Lower probability of enforcement actions. | |
| - Better data security & transparency | Increased confidence in research findings. | |
| - Protected reputation and market value | Avoidance of reputational damage from retracted studies. | |
| - More efficient use of resources | Focus on productive research, not problem-solving. | |
| - Enhanced external image | Making the organization more attractive to partners and clients. |
Experimental Protocols for Contamination Assessment
To build a compelling business case, you need data. The following protocols provide methodologies to quantify contamination levels in your current workflow, establishing a baseline against which the benefits of new investments can be measured.
Protocol: Assessing Labware-Derived Contamination
Objective: To quantify the elemental contamination introduced by pipettes and other labware after different cleaning procedures. Methodology: Based on a study comparing manual and automated cleaning [2].
- Preparation: Obtain 5-mL pipettes (borosilicate glass) and an automated pipette washer designed for parts-per-trillion analysis.
- Cleaning: Manually clean a set of pipettes according to your standard lab procedure. Clean a second set using the automated pipette washer.
- Leaching: Draw an aliquot of 5% high-purity nitric acid through each cleaned pipette.
- Analysis: Analyze the aliquots using ICP-MS for a panel of common contaminants (e.g., Na, Ca, Al, Si).
- Data Analysis: Compare the contamination levels (in ppb) between the manually and automatically cleaned pipettes.
Table 2: Example Results from Pipette Cleaning Study [2]
| Element | Manual Cleaning (ppb) | Automated Washer Cleaning (ppb) |
|---|---|---|
| Sodium (Na) | ~20 ppb | < 0.01 ppb |
| Calcium (Ca) | ~20 ppb | < 0.01 ppb |
| Aluminum (Al) | To be measured | To be measured |
| Silicon (Si) | To be measured | To be measured |
Protocol: Evaluating Laboratory Environment Contamination
Objective: To measure the contribution of ambient laboratory air to sample contamination. Methodology: Adapted from a study comparing regular labs and clean rooms [2].
- Sample Preparation: Place open beakers containing a small volume of high-purity 5% nitric acid in three environments for 4-8 hours:
- Environment A: An "ordinary" open lab bench.
- Environment B: Inside a standard clean hood.
- Environment C: Inside a HEPA-filtered clean room.
- Control: Keep a sealed beaker with the same acid in the clean room.
- Analysis: Analyze all samples via ICP-MS for common airborne contaminants (e.g., Fe, Pb, Al, Ca, Mg).
- Data Analysis: Subtract the control values from the exposed samples to determine the net contamination from the air in each environment (reported in ng/m³).
The Scientist's Toolkit: Essential Materials for Contamination Control
Table 3: Key Research Reagent Solutions for Surface Measurement Research
| Item | Function & Importance |
|---|---|
| High-Purity Water (Type I) | The solvent base for all standards and dilutions; low total matter is critical to avoid introducing a blanket of contamination [2]. |
| ICP-MS Grade Acids | High-purity nitric, hydrochloric, and other acids are essential for sample preparation and digestion. Low elemental blanks prevent skewing trace analysis [2]. |
| FEP/Quartz Labware | Containers made of fluorinated ethylene propylene (FEP) or quartz minimize leaching of elements like boron, silicon, and sodium, which is prevalent in borosilicate glass [2]. |
| Powder-Free Gloves | Powdered gloves often contain high concentrations of zinc and other elements, which can be transferred to samples and surfaces [2]. |
| Certified Reference Materials (CRMs) | CRMs with current expiration dates and known, low contamination levels are necessary for instrument calibration and verifying analytical accuracy [2]. |
| HEPA-Filtration System | Creates a clean-room environment by removing airborne particulates that carry contaminants like iron and lead, which can settle on samples and labware [2]. |
Troubleshooting Common Contamination Problems
Q1: Our ICP-MS results for common elements like sodium and calcium are consistently and inexplicably high across multiple samples. What could be the cause?
- Error: Elevated background levels of common elements.
- Cause: The most common sources are contaminated labware (e.g., pipettes with residual elements from previous use) or poor-quality water and acids used in sample preparation and dilution [2]. Environmental dust in the lab can also be a factor.
- Solution: Implement a rigorous, automated cleaning protocol for all reusable labware. Switch to the highest purity (ICP-MS grade) acids and Type I water. Prepare standards and samples in a HEPA-filtered clean hood or clean room. Run procedural blanks to identify the contamination source.
Q2: We are seeing a specific, persistent contamination signal for elements like zinc or aluminum. Where should we look?
- Error: Persistent contamination with specific elements.
- Cause: Zinc is a common contaminant in neoprene tubing and the powder in some laboratory gloves. Aluminum can be introduced from lab glassware, cosmetics, lotions, or jewelry worn by personnel [2].
- Solution: Replace neoprene tubing with a cleaner alternative like Teflon. Mandate the use of powder-free gloves in the lab. Enforce a strict personal policy of no jewelry, cosmetics, or hand lotions in analytical laboratories [2].
Q3: We opened a new CRM and our calibration is skewed. The CRM is within its expiration date. What might have happened?
- Error: CRM appears contaminated, leading to inaccurate calibration.
- Cause: Surface contamination on the outside of the CRM vial was introduced into the solution during opening, or the CRM was exposed to a contaminated laboratory environment when uncapped [2].
- Solution: Always rinse the outside of the CRM container with high-purity deionized water before opening. Recap CRMs immediately after use to minimize environmental exposure [2].
Visualizing the Cost-Benefit Decision Pathway
The following diagram illustrates the logical workflow for conducting a cost-benefit analysis for a contamination control investment, leading to a data-driven decision.
Conclusion
Addressing surface contamination is a critical, multi-faceted endeavor essential for protecting healthcare workers and ensuring product quality. A proactive approach, integrating foundational risk awareness with advanced methodological detection, effective troubleshooting, and rigorous technology validation, is paramount. The field is advancing towards smarter, faster, and more integrated monitoring solutions, driven by AI, IoT, and standardized immunoassays. Future success hinges on the widespread adoption of standardized guidelines, continued research into tracer drugs and toxicological thresholds, and cross-sectoral collaboration. By embracing these strategies, the biomedical community can significantly mitigate exposure risks, enhance operational safety, and foster a culture of continuous improvement and regulatory excellence.
References
- 1. Safe handling of cytotoxics: guideline recommendations - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4324350/]
- 2. A Common Sense Laboratory Guide to Reducing Errors ... [https://www.spectroscopyonline.com/view/common-sense-laboratory-guide-reducing-errors-and-contamination-icp-and-icp-ms-analysis]
- 3. E. Environmental Services | Infection Control [https://www.cdc.gov/infection-control/hcp/environmental-control/environmental-services.html]
- 4. Hazardous Waste - Decontamination | Occupational Safety ... [http://www.osha.gov/hazardous-waste/decontamination]
- 5. Surface Sampling and the Detection of Contamination - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7152397/]
- 6. Contaminant Help [https://unclineberger.org/tissueculture/contaminant/]
- 7. Assessing Basic Cytotoxic Drug Levels in Hospital ... [https://jhoponline.com/issue-archive/2018-issues/jhop-june-2018-vol-8-no-2/assessing-basic-cytotoxic-drug]
- 8. Worker Safety in Hospitals: Caring for Our Caregivers [http://www.osha.gov/hospitals]
- 9. EU OSHA Hazardous Medicinal Products Update [https://www.equashield.com/articles/eu-osha-update-on-hazardous-medicinal-products-hmps-what-you-need-to-know/]
- 10. Detection and measurement of surface contamination by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4567514/]
- 11. National flu and COVID-19 surveillance report: 22 May ... - GOV.UK [https://www.gov.uk/government/statistics/national-flu-and-covid-19-surveillance-reports-2024-to-2025-season/national-flu-and-covid-19-surveillance-report-22-may-2025-week-21]
- 12. JMIR Public Health and Surveillance - Comparison of Virus Watch... [https://publichealth.jmir.org/2025/1/e69655]
- 13. Best Practices for Contamination Control in Sterile ... [https://www.uspharmacist.com/article/best-practices-for-contamination-control-in-sterile-compounding-outsourcing-facilities]
- 14. High-touch surfaces with moderate contamination levels as ... [https://www.sciencedirect.com/science/article/pii/S0304389425017509]
- 15. When and How to Clean and Disinfect a Facility [https://www.cdc.gov/hygiene/about/when-and-how-to-clean-and-disinfect-a-facility.html]
- 16. High-touch surfaces: microbial neighbours at hand - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7087772/]
- 17. Environmental Cleaning Procedures | HAIs [https://www.cdc.gov/healthcare-associated-infections/hcp/cleaning-global/procedures.html]
- 18. Cross-contamination: A major concern in production ... [https://www.ramblingsaboutdisinfection.com/cross-contamination-a-major-concern-in-production-environments/]
- 19. How to Prevent Cross-Contamination Fast - [https://pharmuni.com/2025/06/08/how-to-prevent-cross-contamination-fast/]
- 20. GMPs 2004 Study: Literature Review of Common Food ... [https://www.fda.gov/food/current-good-manufacturing-practices-cgmps-food-and-dietary-supplements/good-manufacturing-practices-21st-century-food-processing-2004-study-section-2-literature-review]
- 21. Contamination detection by optical measurements in a real ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7065611/]
- 22. The Most Common Contaminants in Food Manufacturing ... [https://blog.aibinternational.com/the-most-common-contaminants-in-food-manufacturing-and-how-to-prevent-them]
- 23. LC–MS Sensitivity: Practical Strategies to Boost Your ... [https://www.chromatographyonline.com/view/lc-ms-sensitivity-practical-strategies-boost-your-signal-and-lower-your-noise-0]
- 24. Contaminants Everywhere! Tips and Tricks for Reducing ... [https://www.chromatographyonline.com/view/contaminants-everywhere-tips-and-tricks-reducing-background-signals-when-using-lc-ms]
- 25. High sensitivity and specificity feature detection in liquid ... [https://www.sciencedirect.com/science/article/pii/S0039914020308717]
- 26. Enhancement of sensitivity and quantification quality in the LC ... [https://pubmed.ncbi.nlm.nih.gov/34997251/]
- 27. Development and Validation of a Simple and Cost-Effective ... [https://pubmed.ncbi.nlm.nih.gov/40509285/]
- 28. Development and Troubleshooting in Lateral Flow Immunochromatography Assays - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7994469/]
- 29. Lateral flow assays - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4986465/]
- 30. Lateral Flow Immunoassay: Methodology, Applications, and Considerations for Use [https://www.jacksonimmuno.com/secondary-antibody-resource/immuno-techniques/lateral-flow-immunoassay-methodology-applications-and-considerations-for-use/]
- 31. A Protocol for the Optimization of Lateral Flow ... [https://bmrat.org/index.php/BMRAT/article/view/788]
- 32. Frontiers | Latest Trends in Lateral Flow Immunoassay (LFIA) Detection Labels and Conjugation Process [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.922772/full]
- 33. A point-of-care diagnostic for drug-induced liver injury ... [https://www.nature.com/articles/s41467-025-61600-9]
- 34. SERS-enabled lateral flow assay for detecting food ... [https://www.sciencedirect.com/science/article/abs/pii/S0889157525009500]
- 35. USP <800> Adds Significant Safety Standards [https://pmc.ncbi.nlm.nih.gov/articles/PMC5398627/]
- 36. Cyber Threats To The SECS/GEM Protocol In Smart ... [https://semiengineering.com/cyber-threats-to-the-secs-gem-protocol-in-smart-manufacturing/]
- 37. Hazardous Drugs—Handling in Healthcare Settings [https://www.usp.org/compounding/general-chapter-hazardous-drugs-handling-healthcare]
- 38. SEMI Standards Information and Control [https://www.semi.org/en/products-services/standards/information_and_control]
- 39. USP <800> : Handling Hazardous Drugs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4252184/]
- 40. New approaches to wipe sampling methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5406133/]
- 41. Using Wipe Sampling to Detect Contamination [https://www.simplivia.com/blog/using-wipe-sampling-to-detect-contamination/]
- 42. Essentials of Surface Wipe Sampling for Pharmacies [https://eagleanalytical.com/updates/essentials-of-surface-wipe-sampling/]
- 43. Hazardous Drug Wipe Sampling: Do I have to? [https://www.pccarx.com/Blog/hazardous-drug-wipe-sampling-do-i-have-to]
- 44. A scoping review of surface wipe sampling for ... [https://pubmed.ncbi.nlm.nih.gov/40305371/]
- 45. Sampling | US EPA [https://www.epa.gov/hw-sw846/sampling]
- 46. Wipe sampling of antineoplastic drugs from workplace ... [https://www.sciencedirect.com/science/article/pii/S2773049224000023]
- 47. Development and validation of a quantitative wipe ... [https://pubmed.ncbi.nlm.nih.gov/38835271/]
- 48. Creating and Implementing A Hazardous Drug Wipe ... [https://www.eurofinsus.com/environment-testing/built-environment/resources/recent-news-blogs/blog-hazardous-drug-wipe-sampling-plan/]
- 49. Evaluating surface contamination at hazardous waste sites [http://www.osha.gov/hazardous-waste/surface2]
- 50. Monitoring contamination of hazardous drug compounding ... [https://www.sciencedirect.com/science/article/pii/S1130634323005664]
- 51. A Guide to Environmental Monitoring [https://www.eurofinsus.com/food-testing/resources/a-guide-to-environmental-monitoring/]
- 52. How should environmental monitoring locations be chosen? [https://www.europeanpharmaceuticalreview.com/news/170511/how-should-environmental-monitoring-locations-be-chosen/]
- 53. Evaluation of a hazardous drug surface contamination ... [https://pubmed.ncbi.nlm.nih.gov/39953987/]
- 54. Evaluating Monitoring Strategies to Detect Precipitation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5703154/]
- 55. Monitoring Surface Contamination of Hazardous Drugs ... [https://www.ons.org/publications-research/voice/news-views/10-2018/monitoring-surface-contamination-hazardous-drugs-and]
- 56. Water Quality Sampling Frequency Analysis of Surface ... [https://www.frontiersin.org/journals/sustainable-cities/articles/10.3389/frsc.2021.791595/full]
- 57. Sterilization, Disinfection, and Decontamination [https://researchsafety.gwu.edu/sterilization-disinfection-and-decontamination]
- 58. Principles of decontamination, sterilization, and disinfection [https://www.selectagents.gov/compliance/guidance/biosafety/appendix1.htm]
- 59. About Hierarchy of Controls [https://www.cdc.gov/niosh/hierarchy-of-controls/about/index.html]
- 60. CCOHS: Hazard and Risk - Hierarchy of Controls [https://www.ccohs.ca/oshanswers/hsprograms/hazard/hierarchy_controls.html]
- 61. Engineering Controls for Laboratory Safety [https://blink.ucsd.edu/safety/research-lab/laboratory/engineering.html]
- 62. Controlling Cross-Contamination in Research Facilities [https://dycem.com/blog/controlling-cross-contamination-in-research-facilities/]
- 63. Guidelines for preventing and reporting contamination in ... [https://www.nature.com/articles/s41564-025-02035-2]
- 64. Chapter 4 - Administrative Controls [https://ehs.cornell.edu/book/export/html/1050]
- 65. Chapter 2 - Engineering Controls [https://ehs.cornell.edu/research-safety/chemical-safety/laboratory-safety-manual/chapter-2-engineering-controls]
- 66. Cleaning Validation: 8 Steps for FDA Compliance Success [https://zamann-pharma.com/2024/07/17/cleaning-validation-7-steps-for-fda-compliance-success/]
- 67. Cleaning validation protocol for pharmaceutical industry [https://www.gmpsop.com/cleaning-validation-protocol/]
- 68. Validation of Cleaning Processes (7/93) [https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/inspection-guides/validation-cleaning-processes-793]
- 69. addressing false positives, false negatives, and base rate ... [https://link.springer.com/article/10.1007/s00477-024-02898-7]
- 70. AI for Human Error Detection in Manufacturing [https://www.orcalean.com/article/using-ai-to-spot-human-error-patterns-across-shifts-and-plants]
- 71. Preventing intense false positive and negative reactions ... [https://www.sciencedirect.com/science/article/pii/S0022175914000878]
- 72. Mapping global floods with 10 years of satellite radar data [https://www.nature.com/articles/s41467-025-60973-1]
- 73. Industrial Training Approaches to Reduce Human Error ... [https://www.gpstrategies.com/blog/industrial-training-reduce-human-error/]
- 74. Limit of Blank, Limit of Detection and Limit of Quantitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556583/]
- 75. What is the difference between Limit of Detection (LOD) ... [https://lab-training.com/difference-limit-detection-lod-limit-quantification-loq/]
- 76. What is the difference between Limit of detection (LOD) and ... [https://blog.quality-pathshala.com/2023/08/10/what-is-the-difference-between-limit-of-detection-lod-and-limit-of-quantification/]
- 77. Binding the gap between experiments, statistics, and ... [https://www.sciencedirect.com/science/article/pii/S0003267021011685]
- 78. Comparison of approaches for assessing detection and ... [https://www.nature.com/articles/s41598-024-83474-5]
- 79. Strategies for Achieving the Lowest Possible Detection ... [https://www.spectroscopyonline.com/view/strategies-achieving-lowest-possible-detection-limits-icp-ms]
- 80. LOD, LOQ, MDL, and PQL: The Driving Force of the Next ... [https://advancedplatingtech.com/technical-library/plating-topics/lod-loq-mdl-and-pql-the-driving-force-of-the-next-generation-of-regulations/]
- 81. Limit of detection (LQD)/limit of quantitation (LOQ) [https://pubmed.ncbi.nlm.nih.gov/8013092/]
- 82. statistical uncertainty near the detection limit [https://pmc.ncbi.nlm.nih.gov/articles/PMC5907527/]
- 83. Bayesian optimization of the conditions for highly sensitive ... [https://pubs.rsc.org/en/content/articlelanding/2023/ja/d3ja00195d]
- 84. Immunoassays: Analytical and Clinical Performance ... [https://www.mdpi.com/1422-0067/25/4/2080]
- 85. Mass Spectrometry in the Clinical Laboratory—Challenges ... [https://www.spectroscopyonline.com/view/mass-spectrometry-clinical-laboratory-challenges-quality-assurance]
- 86. Advances in environmental pollutant detection techniques [https://www.sciencedirect.com/science/article/pii/S0160412025001163]
- 87. Recent Advances in the Detection of Food Toxins Using Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10731662/]
- 88. Catch us at ASMS2025 - PAL System [https://www.palsystem.com/en/newsroom/news/asms2025/]
- 89. Comparative evaluation of four new immunoassays and LC ... [https://pubmed.ncbi.nlm.nih.gov/40584217/]
- 90. Advances in research on novel technologies for the ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1658241/full]
- 91. Review Advances in mycotoxin detection techniques and ... [https://www.sciencedirect.com/science/article/pii/S0278691525001541]
- 92. Comparison of calibration results for α, β surface ... [https://pubmed.ncbi.nlm.nih.gov/39656632/]
- 93. Research on contamination-aware adaptive calibration ... [https://www.sciencedirect.com/science/article/abs/pii/S1350449525004852]
- 94. How Often Do Radiation Instruments Need To Be Calibrated? [https://www.radsafety.com/how-often-do-radiation-instruments-need-to-be-calibrated]
- 95. Radioactive standards and calibration methods for ... - INIS-IAEA [https://inis.iaea.org/records/017yj-cde52]
- 96. Instrument calibration procedure for pharmaceutical industry [https://www.gmpsop.com/instrument-calibration-procedure/]
- 97. Multicenter Study Shows U.S. Hospitals Vary Greatly in ... [https://www.hopkinsmedicine.org/news/newsroom/news-releases/2025/09/multicenter-study-shows-us-hospitals-vary-greatly-in-how-they-define-blood-culture-contamination]
- 98. Standardized surveillance of blood culture contamination rates [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506060/]
- 99. Cell Culture Contamination Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination?srsltid=AfmBOoooDegfn7-9xvAoh6wkM-f56Vc068rdKjHQK89lhrU5Fha0rxNl]
- 100. What is a cost-benefit analysis (CBA)? [https://www.atlassian.com/work-management/strategic-planning/cost-benefit-analysis]
- 101. Analyze Costs, Benefits and Risks Associated with Each ... [https://www.oceg.org/projectriskleader/step-8-analyze-costs-and-benefits-associated-with-the-plan/]